An incentive is something that motivates an individual to perform an action.
And, that something could be anything. Meet the omnipresent influencer of behavior. Frequently, incentive is understood to be associated with some form of monetary compensation for specific behavior. But, incentives are not merely monetary. And, they exhibit influence. Yes. Always. 100% of the time. In any environment, any scenario, any interaction, and every decision including clinical encounters. Incentives can be viewed as any tangible or intangible reinforcement, and thus influencer, of behavior. Theses “rewards” range from monetary to personal, concrete to cognitive-emotional. And interestingly, incentives still affect behavior even when individuals consciously identify and recognize their presence. They are social, contextual, or even cultural. And, they impact decisions and performance.
Incentives are present in a variety of forms and contexts. Most generally, incentives can be assessed via a variety of binary comparisons including: Explicit verses Implicit, Reward verses Punishment, Short verses Long Term, and Immediate verses Delayed. Yet, the content of incentives range from monetary to verbal, and in contexts of private and public. The environment, including people, specific location, and context of the situation, in conjunction with broader constructs such as expectation and culture also matter.
Physician’s prescribing habits are affected by pharmaceutical marketing. Prescribing is affected by the gifts, no matter how menial, of pharmaceutical companies. This effect is observed even if physicians believe the gifts have no bearing on their prescription decisions. The data and incentives lead the Office of the Inspector General to research gifts and payments that promote prescription drugs. In this instance, physicians are Prescribing Under the Influence:
This kind of advertising is crucial to sales. A doctor is not going to prescribe something he or she has never heard of, and it’s the drug representative’s job to get the products’ names in front of the physicians. Maybe the drug representative does that while the resident is slathering cream cheese on a bagel; maybe it’s while the intern is saying, “Oh, what’s this cute little stuffed bear?” Either way, the doctor stops and spends a moment.
In private practice, the little gifts are often even more important. If you’re a drug representative, physicians are usually not interested in talking to you unless you have something to catch their attention. Then you can get your three sentences in: “We’ve got such and such on the hospital’s formulary now.” Or “The new form of this drug can be given once a day instead of four times a day. The patients will love it.” It’s a way to get in the door so that your information rather than somebody else’s reaches the doctor’s brain.
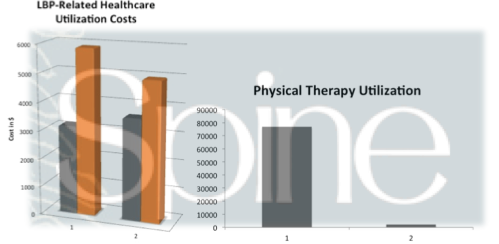
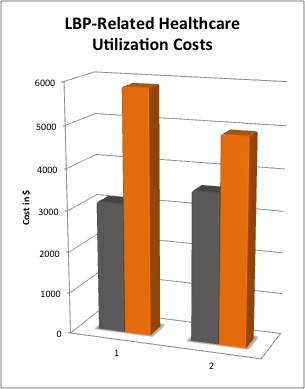
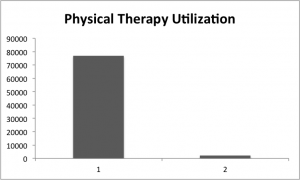
Self-referral, or referral for profit, is associated with increased utilization of lab tests, imaging, and physical therapy. A meta-analysis revealed a 2.48 combined relative increased frequency of referral in refer for profit scenarios. In most cases, I truly believe physicians are not sitting in front of patients actively scheming on how to justify an imaging procedure, lab test, or referral to physical therapy in order to maximize profit. On the whole, I don’t assume the physicians in these scenarios are unethical and overtly over prescribing. But, the incentive is present, and thus behavior is altered. The evidence shows that self-referral invariably leads to higher utilization and higher costs.
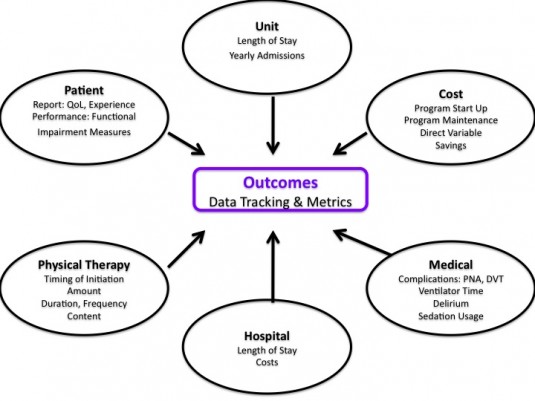
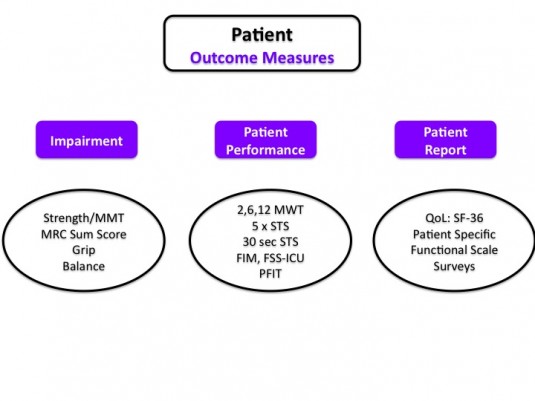
What are specific incentives within the profession of physical therapy? What should be modified? Everyday outcome measures are handed to patients, clinical measurements made, and assessments written. What are patients and incentivized to say and do? Or, believe? Administrators, managers, and clinic directors in hospitals and private clinics present data to their staff. Specific metrics are identified and goals are constructed.
Recognizing the development of interaction between personal and environmental (including social, societal, cultural) influences on behavior illustrates the complexity of how, when, and why we behave in certain ways. In healthcare, the layers of systems and hierarchy of influence is complicated. Our decisions and behavior are not nearly as rationale, nor conscious, as they feel to us personally. The interplay of personal, inter-personal, and environmental influences coupled with tangible or perceived rewards influences how people act. In conjunction with individual motivation, incentives, both seen and unseen, are determinants of who will thrive in certain educational and clinical contexts. One such example is the difference between extrinsic and intrinsic motivation. What people do is just as complex as why people think they do it. And, there is a disconnect, a blind spot, between our perception of bias in ourselves verses others.
Unfortunately, incentives have unintended consequences. The cobra effect is an illustration that “incentives don’t always work out the way we expect them to.” Beyond identifying a target metric and outcome, it’s imperative to identify the actual behaviors that are desired. Sometimes a change in a specific measurement (productivity, patient report outcomes, etc) do not necessarily reflect the desired behavior changes. In particular, research investigating payment incentives and subsequent clinician behavior within healthcare illustrate tangible manifestations of “unintended consequences.”
How is the outpatient therapist incentivized if measured and assessed primarily via patient report questionnaires? How are we changing behavior in the acute care therapist by assessing them based on the number of “units” they “bill?” What about the outpatient therapist who receives a bonus based upon units billed? What if changes in the metrics we are utilizing don’t truly illustrate significant change, don’t result in the best care, and don’t reinforce ideal behavior? A health services research article on medicare payment comments:
While some payment methods may lead to excessive utilization, other payment methods may put too much pressure on cost containment and potentially lead to underprovision of resident care (Coburn et al. 1993; Cohen and Spector 1996; Murtaugh et al. 1988)
In addition to tracking specific measures, ideal behaviors need to be identified. To account for unintended consequences broadly identify various behaviors likely to lead to the measured goals. Sometimes behaviors that are actually not desired can cause significant desirable change in target measures. Undesirable action for desired outcome. So, what behaviors can cause a change in the metric? And, what contributes to encouraging such behaviors? But, also, what incentivizes behaviors that change the metric, but may also cause unintended consequences?
If a clinic, hospital, profession, or health care system seeks to fundamentally alter care delivery robust assessment of the current incentives within healthcare, including conflicts of interest is mandatory. Then change the incentives to affect and encourage ideal clinician behavior. A successful approach likely involves a combination of incentivizing important outcomes as well as specific behaviors. Changing the single data point does not necessarily reflect the desired overall change in other measurements or behavior. The depth of affect of incentives in conjunction with unintended consequences illustrate the difficulty in controlling change. A seemingly brilliant idea such as “pay for performance” or outcomes based payment is fatally flawed without a conscientious focus on the many potential behaviors that may result in the specific outcome. Might it even be chaos?
What are the incentives? Identify the answers and then target behaviors requiring alteration. Shift behaviors towards ideal processes. Ideal behaviors will likely have positive unintended consequences. A myopic focus on only the desired numeric change will produce a myriad of potentially paths to “success.” Some of these paths were never the intended action of success. And in fact, may be the opposite of the incentive’s initial philosophical goal.