If immobility is pathology, then movement is medicine. But, now that the rationale is present, how is action initiated? Understanding the current literature in regards to mobility and physical therapists in the intensive care unit illustrates the need and the potential for physical therapists. This potential leads to the vision. Yet, rationale and vision do not guarantee action, nor results.
Every patient requires an individualized assessment and interaction to determine the best plan of care, outcomes tracking, and goals. So, does each individual ICU. Evaluation of current practice and culture, barriers to mobility and physical therapy, and a plan to achieve specific goals. Data and outcomes tracking can provide insight into progress.
Research surveying various professions elucidates commonly reported barriers to mobility and physical therapist involvement in the ICU. Yet, many of the identified barriers appear more perception than the reality. Fears based upon “what if?” scenarios. What if the patient falls? What if a line becomes dislodged? What if they decompensate? What’s the worst possible event? Illness severity, safety, and line dislodgment are commonly report. These fears are contrary to the literature on safety and feasibility. Does this indicate these concerns are likely unwarranted?
Barriers: Perception and Reality
Perception is reality. The multi-disciplinary environment of critical care, including the a culture of a specific unit, requires analysis to ensure specific perceptions are identified. Barriers should be overcome with education, discussion, training, and graded exposure. Individual practitioner’s perceptions, fears, and concerns contribute to professional interactions, unit culture, and ultimately patient care. Fear based barriers include illness severity, illness acuity, safety, feasibility, and perceived lack of benefit. Other reported challenges include lack of consults, staffing, knowledge, time, expertise, experience, cost, equipment, and unit culture. All unit specific and individually identified barriers must not only be acknowledge, but adequately addressed. Reported concerns are not to be discounted.
Perceptions
- Illness Severity
- Illness Acuity
- “Too Sick”
- Unsafe
- Not Feasible
- Lack of Need
- Lack of Benefit
Logistics
- Time
- Equipment
- Lack of Consults
- Lack of Priority
- Staffing
Culture, Practice Patterns, & Professional
- Knowledge of Individuals & Various Professions
- Experience & Expertise
- Sedation
- Current Mobility
- Current Physical Therapist Presence & Practice
Now, this of of course is not an exhaustive list. A unit may contain unique barriers and perceptions outside of this list. Focused meetings, targeted surveys, and small group discussions can assist in illuminating the beliefs of individuals and the overall culture of a unit. A physical therapist lead quality improvement project to promote early mobility in the intensive care unit utilized a survey of nurses and respiratory therapists to identify current perceptions.
1. Do you think physical therapy should evaluate/screen all intensive care unit/cardiovascular intensive care unit patients?
2. Do you feel comfortable getting patients into neuro chairs without physical therapy?
3. Do you feel comfortable using the mechanical lifts without physical therapy?
4. Do you get patients out of bed/ambulate without physical therapy if they are able?
5. Do you think patients should be getting up on ventilators?
6. What are the barriers to mobilizing patients on ventilators?
7. What are the harmful effects of physical therapy working with patients in the intensive care unit?
8. What can physical therapy do to improve communication with the RNs, MDs, respiratory therapists, patients, families, etc.? Please be specific.
9. What can physical therapy do to improve patient care? Please be specific.
The survey questions revealed many of the barriers listed above. Interestingly, all respondents agreed that every patient in the ICU should be evaluated by a physical therapist.
As much, as soon, as often as we can?
The concept of mobility and rehabilitation during intensive care appears quite important and profound. Therefore, it’s quite obvious that every patient should be out of bed and ambulating at least three times per day. Well, not exactly. Although being in the ICU in the presence of lines, tubes, and life support equipment should not automatically preclude individuals from movement and therapy participation, each patient will present and perform quite differently.
So, what are the specific interventions? How does a physical therapist decide what to do? And, when? What about dosage, intensity, frequency, and duration? Similar to other patient populations (such as individuals with back pain), critical illness is far from homogenous. Even a very specific ICU type contains a range of diagnoses and individuals. Treatment content, duration, intensity, and frequency should likely vary. Further, given the acuity of illness and the medical complexity of patients, close monitoring of many variables is necessary. The specifics of these particular concepts remain complicated and dependent on many variables. At times it appears there are more questions than answers.
Generally, the goal is to decrease sedation, bed rest, and confusion while increasing wakefulness, movement, and engagement. There are nearly infinite options available to accomplish such goals. An approach of “as much, as soon, and as often as possible” simplifies the conceptualization of treatment. But, such an approach is always performed within the specific confines and constraints of the system, staffing, experience, and culture of the current clinical situation.
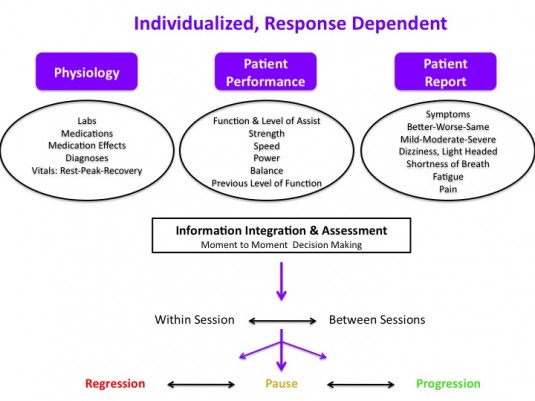
Response Dependent Progression
An individualized, response dependent approach facilitates proper monitoring from moment to moment and session to session. Decision making requires integration of information from multiple sources to reach an overall assessment that determines progression, pause, or regression. Such a system hopefully decreases the likelihood of grossly “over treating” or “under treating” a specific patient at each specific encounter. The variable nature of medical stability, presentation, and physiologic status of critical ill patients may result in robust, swift changes in vital signs, physiology, and even patient performance. A patient’s specific clinical scenario including diagnoses, physiologic state (labs, medications, vital signs), and current medical goals warrants the a priori construction of individualized safety parameters regarding upper and lower limit values for vital signs.
The research to date suggests that in order to achieve maximum effect physical therapy should be performed in the ICU, while patients are intubated, 5-7 days a week, and in conjunction with or following sedation interruption. Initiate a progressive approach focused on achieving functional milestones such as sitting, standing, marching, transferring out of bed, and ambulating as quickly, but as safely as possible. Exercise testing, prescription, and progression is feasible, effective, and possibly predictive. Although, given the duration of bed is associated with weakness and long term physical impairment suggests functional mobility should likely not be neglected.
Measuring, Assessing, & Planning
An assessment of current and historic practice can include average unit census, average number of physical therapy consults, percent of the unit with consults, and number of patients actually seen per day. Average time from admit to first physical therapy encounter in conjunction with average duration and frequency of treatment provide general insights into current physical therapy practice.
Next, by assessing unit specific data in relation to current practice, predictions for future staffing, equipment, and training can be constructed. Such a model can be further specified based upon targets for the number of patients (or percentage of the unit) to be treated each day, and at what frequency. In addition, the current number (or percentage of) patients who are likely to benefit from, or be appropriate to participate in, physical therapy can illustrate a disconnect between current practice and ideal practice. Identifying a lack of consult standards may shed light on variability in consult numbers, timing, and frequency. Standardized criteria for consults, mobility, or physical therapist involvement provide assistance in decision making. But, each individual patient requires analysis within the framework of guidelines, not decisions mandated by them.
The current demand (consults), physical therapy practice, and provider perceptions are utilized to model need, illustrate the lack of physical therapist involvement, and potentially quantify a current lack of resources to provide appropriate timing, frequency, and duration of therapy. If feasible, informal or formal investigations into factors associated with physical therapy consultation provide further understanding into current practice regarding physical therapy consultation and practice. A disconnect between the research literature and current unit culture, including various professions practice patterns, highlights the need for transdisciplinary practice change and potential quality improvement.
Financial Modeling
Johns Hopkins constructed a financial model allowing prediction of staffing, costs, and potential financial outcomes. By utilizing the number of yearly admits, current ICU & hospital length of stay (for a specific targeted ICU), and direct variable costs of care a very accurate model of staffing, start up costs, and potential cost savings scenarios can be assessed. Varying possible length of stay reduction outcomes allows for a sensitive, yet conservative prediction of cost savings in multiple potential situations. Modeling various outcomes allows for the presentation of worst case, likely, and best case end points. Utilizing actual data from their own quality improvement project and data from the literature they conclude
A financial model, based on actual experience and published data, projects that investment in an ICU early rehabilitation program can generate net financial savings for U.S. hospitals. Even under the most conservative assumptions, the projected net cost of implementing such a program is modest relative to the substantial improvements in patient outcomes demonstrated by ICU early rehabilitation programs.
Measurement and Outcomes Tracking
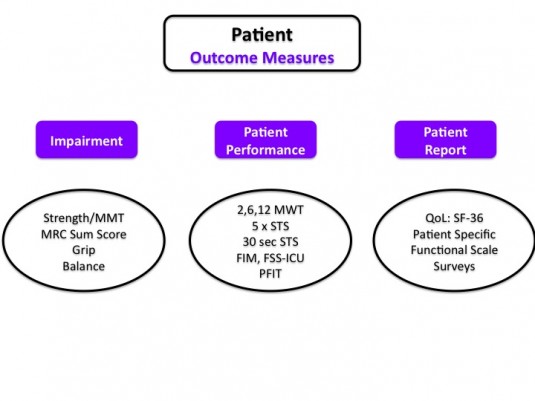
The potential data and outcomes depend on data availability, program goals, ICU type, patient population as well as any specific research questions. Outcomes can be analyzed at the patient, unit, and hospital level.
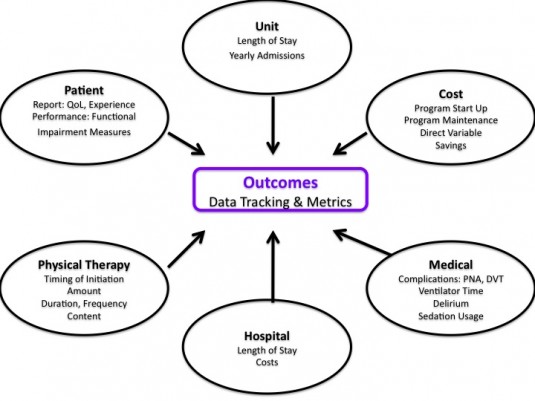
At the patient level there are a variety of impairment, patient report, and patient performance measures, many of which have been specifically investigated for utilization in the intensive care unit.
Quality Improvement Project Design
Designing and implementing a quality improvement project with a focus on research methodology improves the accuracy of measured results. Such an approach eases discussions with hospital administrators regarding need, costs, and program appraisal. Appropriate planing, background research, and project construction prior to implementation allows for more specific analysis.
Background, Construction, & Education
- Assess current PT practice, unit culture, clinician perspectives
- Compare current practice to ideal practice, current program models, and feasible quality projects
- Construct project goals
- Model staffing, training, equipment, and program requirements
- Identify, acknowledge, and address current barriers
- Identify champions from each discipline: PT, RN, MD, RT
- Interdisciplinary Meetings & Education: RT, RN, MD, RT
- Acknowledge, educate, address concerns
- Join Critical Care Quality Meetings or Committee
- Identify Lead PT for ICU(s)
- Assign ICU Unit Based Physical Therapist(s)
- Identify educational needs of PT and rehab department
- Identify educational needs of other disciplines
- Perform education and follow up meetings
Data
- Identify target data and outcomes tracking
- Obtain facility specific data for financial modeling
- Build data tracking sheets & data bases (if needed)
- Leverage electronic medical record (if able)
- Train clinicians on documentation and “data entry”
- “Go live” with documentation and data collection
- Establish a post documentation training pre-project implementation baseline
Implementation
- “Go Live”
- Sustain & Maintain Program via Updates and Meetings
- Evolve care based on observation, feedback, and data analysis
- Assess & Analyze Program and Data Collected
The elegance of a quality improvement approach is the potential for an ever evolving feedback loop of assessment, planning, implementation, and analysis. At specified intervals, repeat the process based on current results, identified issues, and current research.
Facility Specific Questions and Issues
1. What if current practice illustrates a lack of consults, infrequent consults, or poor timing of consults (i.e. too late in hospital course)?
Create specific consult criteria. Educate nursing staff and physicians. Provide checklist.
2. What if there is no dedicated physical therapist in ICU?
Quality improvement project focused on unit based physical therapist and increased overall patient mobility.
3. What if patients are too sedated?
Assess RN sedation guidelines and practices. Pair therapy with sedation vacations & awakening trials. Meet with MD’s, RN’s, and RT’s. Work with RN educator to facilitate RN lead project regarding sedation.
4. What if there is a lack of patient mobility outside of therapy sessions?
Nursing staff education. Nurse targeted progressive mobility guideline.
5. How to prioritize if unable to address every consult and patient on caseload in the ICU(s)?
Focus on duration of bed rest, individuals requiring mechanical ventilation, especially those requiring greater than 3 days of mechanical ventilation. Assess last time mobilized and last therapy session.
Quality and Assessment
Obviously, analyzing and interpreting clinically generated data is difficult. Given the complexity of the daily clinical environment and lack of rigor available in a controlled research trial, data can often be inaccurate or even misleading if not understood properly. Utilizing a quality improvement model within the context of critical care is an evolving method for program design and interpretation, but
The results of many quality improvement (QI) projects are gaining wide-spread attention. Policy-makers, hospital leaders and clinicians make important decisions based on the assumption that QI project results are accurate. However, compared with clinical research, QI projects are typically conducted with substantially fewer resources, potentially impacting data quality…Data quality control is essential to ensure the integrity of results from QI projects.
Resources exist for appropriate design, training, data collection, implementation, sustainability, assessment, analysis, interpretation, and translation of quality improvement designs and data.
1. The SQUIRE (Standards for Quality Improvement Reporting Excellence) guidelines for quality improvement reporting: explanation and elaboration
2. Intensive care unit quality improvement: a “how-to” guide for the interdisciplinary team
3. Improving the quality of quality improvement projects
4. Improving data quality control in quality improvement projects
5. How to use an article about quality improvement
6. Rehabilitation quality improvement in an intensive care unit setting: implementation of a quality improvement model
7. ICU early physical rehabilitation programs: financial modeling of cost savings
8. Translating research into clinical practice: the role of quality improvement in providing rehabilitation for people with critical illness
9. Quality Improvement Guide

Hello,
I have very much enjoyed your last few posts. I am an acute therapist at a large hospital in the NW. I spend a lot of time advocating for early mobility and PT in the ICU. I want to share this information with my supervisior, would it be ok to contact you with any follow up questions? Thank you for sharing your work.
Lauren