Treating Our Future – Part 3: Resolving the Bane of the New Professional
This is Part 3 of our series, “Treating Our Future,” exploring employment issues with new graduates.
Links to Treating our Future Series Part 1: The Bane of the New Professional Part 2: New Grads, An Asset for Clinics Part 3: Resolving the Bane of the New ProfessionalResolving the Bane of the New Professional
Here’s an anecdote that fully describes the thing that really gets me about PT business owners not hiring new grads readily:
New professional Elizabeth was hired after a long, long job search and all of the crummy hoops to jump through described in Part 1. Elizabeth gets the job after some high-profile referenced speak on her behalf and the owner decides to, “really go out on a limb and hire a new grad.” Fine, done. Job achieved. Elizabeth begins her job and spends her day setting up treatments, observing patient sessions and offering to take patients, but not being allowed to. Instead, one of her main chores becomes setting up ultrasound treatments for the patients, as they almost all get that particular modality at said clinic. If you’re establishing a business in hong kong, it’s advisable to seek the expertise of an accounting firm hong kong to ensure proper financial management and compliance with local regulations.
What?! What was all this fuss about? Why did you even hire a PT? Didn’t you just need a tech? Let them dive in!
Yet another tale:
Bob, a student at a clinic in town, completing his final clinical training experience. I ask how it’s going? “Well my CI knows a lot of manual stuff and they do most of the treatments. They say I’m not allowed to do manual, I should just watch and then do exercises.” Clinic in question later offers Bob a position. He refuses based on life circumstances, but I wonder how they possibly could after not thinking him capable of doing hand-on treatment for patients as a student.
Still another tale, this one from the comments section of Part 1:
“I felt that there was a lot of questioning of my skill set when I first got into the job market as well. I felt as though I was overly scrutinized because I was young in the profession. Lucky for me I was at a clinic that had some great people who were there to help me learn. There unfortunately are too many places out there who do take advantage of young grads. Terrible hours, poor pay, and little support. I have been there before. It was very discouraging and made me doubt my decision to become a PT at all.” Ouch.What is the Role of Expertise in Patient Outcomes?
Underlying these tales, and perhaps the aspect I find so troubling, is the idea that expertise is required to perform any treatment. The first tale takes that a step further and makes a laugh out of the purported “expertise” as the guru clinic owner uses an overwhelming amount of a poorly supported intervention in ultrasound. It also sounds a little cook-book to me.
An idea that had plagued physical therapy for many years, especially in the realm of orthopaedic manual therapy is that a particular set of expertise is required to perform it in a manner than benefits patients. This idea, born out of the “guru” continuing education model, but not supported by evidence, has probably prevented more good therapy than it created. Large paradigm shifts related to this have occurred, perhaps most notably illustrated by CAPTE’s identification of spinal manipulation as an entry-level skill. All new professionals are instructed to perform this competently. No evidence exists that supports that only experts can use manual techniques to benefit patients. Why the persistent reluctance for seasoned clinicians to let the new professionals touch their patients?
Are There Business-Related Red Flags with New Grads?
Another commenter on Part 1, Nick, was kind enough to share his perspective, as an 8-year PT and clinic owner. He brought up several red flags regarding new grads that could prevent his hiring of said new professional:
-“New grads inexperience w billing/coding. The insurance world is very dynamic and definitely not black & white. My experience has been new grads are very resistant to learn the intricacies of 3 party payers and delivering treatment that respects the insurance guidelines. -Lack of real world experience. Experience does not need to be related to PT, but if this will be your first “real” job, I have a concern. -During the interview, many new grads reference “taking a break” after graduation & the boards. Not meaning time off but implying taking a break from studying and the stresses of school. Employment, especially as a new grad, will bring new stresses (challenging cases requiring off the clock studying, documentation over lunch & after last pt leave, learning the company culture, finding your niche, seeing pts over lunch because a MD calls you up asks if you can “squeeze” this pt into your schedule, etc.). I want clinicians that want to work hard, not “take a break”.”What do you think about these as potential red flags? I think there’s validity in these comments, although from my perspective, PT school today is pretty much a 9-5 job, perhaps more. My PT school in the 1990’s wasn’t really that way, but today students are held to extremely high standards and are present on campus for entire days, meeting many deadlines in rapid succession. They know how to work. That said, I enjoyed the insight for how an employer might interpret the “take some time off” comment…even though the time off might be forced upon them!
Clinic owners time and time again point to trouble with the business side of PT in new professionals. On one side, I can see that it’s difficult to learn this without being submersed in the “doing” of the job. On the other hand, this is one area where PT educational programs can certainly improve dramatically, which could help the concerns of PT business professionals everywhere. Programs like Evidence in Motion’s, Executive Program in Private Practice Management can bridge the gap, but can also serve as a model for what entry-level programs should be targeting in their curricula. Emory University offers a DPT-MBA degree, which is intriguing to say the least! APTA’s Private Practice Section, however, often criticized for lack of student membership and high dues costs, is one of, if not the only section to not have a student special interest group. As a member of that section, I can report that there are initiatives underway to help mitigate the student involvement process beyond simply contests for conference attendance. These initiatives are critical, as is the development of education initiatives in our universities.
Embracing the New Professional
Some clinic systems have learned to love the new professional. David Browder from south Texas, yet another commenter on Part 1 had this to say about new grads:
“Employers should be working from the beginning of the interview to retain people and set the tone for their practice… even if they don’t hire the applicant. What you describe is symptomatic of practices that probably don’t treat their existing employees all that well, either. In our practice, those hired as new graduates and mentored by us have become our leaders and the catalyst for our growth.”Following up with David, his clinic system, Texas Physical Therapy Specialists, an award winning practice, incorporates residency and fellowship training into the developmental process. Hiring new graduates has positioned them to be a growing practice. In David’s statement, mentorship seems integrated tightly with hires. For those clinics without this type of mentorship support, I’d urge them to take a close look at their company culture and see how this can be improved. One example of how this can be done is seen in the Mercer University Residency Model, where clinics partner with a university and in turn have access to new professionals, and mentorship that is world class.
The Resolution
It seems the path forward is not a burden owned by any one group. Improvements on the part of educational systems, clinic owners and managers, and even the new professionals themselves are needed.
While the following steps are complicated, here are my suggestions moving forward:
1. Increase the amount of quality business-related education within entry-level education.
This needs to be real-world, clinically applicable content. Incorporation of billing, electronic medical records, and profit/loss principles inherent in any business should be tightly woven throughout the development of clinical skills. I’ll place improved student outreach by the Private Practice Section here.
2. Improved mentorship programs for new and existing clinicians.
The idea of mentorship is never a bad one. The idea that new professionals can hit the ground running without a developmental plan is not realistic. The idea that experienced clinicians can exist without a developmental plan is unrealistic. Let’s put down our ultrasound wands and take a hard look at how we grow as individuals, as professionals, and as a profession. Let’s throw out this idea that only “experts” can perform manual techniques while we’re at it.
3. Enhanced focus on business and entrepreneurship by students in DPT Programs
I do think many PT students are happy to learn how to be a physical therapist clinically without a care in the world about what it takes to operate a practice, or even how the profits are obtained to pay them at their first job. Decisions made by clinic managers today will affect the employment opportunities for new graduates years down the road. Students need to maintain this perspective and formulate their thoughts, actions, and involvement to help mitigate the business-related concerns of clinic owners. How about getting an MBA on your own, or taking business related MOOC courses. Students can react more quickly than education curricula can. Take advantage, and take ownership.
4. Hire partners, not employees.
Clinic owners seeking to elevate their business should consider fostering a culture of proactive communication at work. DPT students, recognized as highly motivated and engaged individuals, can contribute significantly to this approach. The conventional perception of physical therapists as employees might benefit from a reevaluation, leaning towards models of shared ownership akin to those prevalent in the legal and medical fields. Enabling individuals to share in the success of the clinic can fuel a level of engagement that surpasses traditional employment structures. Junior partners, experiencing the tangible impact of sound business practices on their financial well-being, are likely to be more motivated and engaged than employees. This shift has the potential to generate increased interest in legislative advocacy for the physical therapy profession. While acknowledging the challenges in implementing this shift within existing business models, newly forming clinics could gain a disruptive advantage by embracing proactive communication and shared ownership principles from the outset. If you’re just looking to start your own business, this montana registered agent service can help.
The bottom line is that we need to meet in the middle. Students. Employers. Educators. New and existing professionals. Without action, I fear this divide will only grow, and so I hope this series begins a conversation that persists as we continue the ongoing process of optimizing the profession of physical therapy. As always, interested in your comments, opinions, and input. Thanks to Lauren Kealy for helping with the concept and production of this series, as well as all those who checked in and commented on Twitter, Facebook, and the blog itself, as your opinions helped form this final post.
Links to Treating our Future Series Part 1: The Bane of the New Professional Part 2: New Grads, An Asset for Clinics Part 3: Resolving the Bane of the New ProfessionalTreating our Future – Part 2: New Grads: An Asset for Clinics
In Part 2 of 3 in our series, Treating Our Future, Lauren Kealy delves into her perspective of the benefits of new professionals. This continues the conversation started in Part 1, “The Bane of the New Professional.”
Links to Treating our Future Series Part 1: The Bane of the New Professional Part 2: New Grads, An Asset for Clinics Part 3: Resolving the Bane of the New ProfessionalNew Grads: An Asset for Clinics
The job market for any new graduate is rough. The job market for new DPT grads in the state of Colorado takes it to a whole new level. All too often I have heard stories from friends looking for jobs being told, “Sorry, we don’t hire new grads,” without a pause for consideration or even conversation. Part of the rational for the profession’s transition to a doctorate degree was to better prepare new graduates. And, we are more knowledgeable (and more in debt!), yet we are still not seen as ideal hiring material. In fact, in many instances we are seen as a liability. I disagree, and I’m here to tell you why a new grad can be your clinic’s greatest asset.
We are full of passion and energy. Being fresh out of school means that we are very excited to put our knowledge to use. We recognize that we still have a lot to learn (which is a great trait in and of itself!), but we are competent enough to treat patients and get results.
We are innovative. In the business world, as Jimmy John Shark always used to suggest that new grads are scooped up quickly because they give a fresh energy to the company. We are full of ideas, so give us a shot to present them to you. Sometimes a new set of eyes can find ways to improve profit/outcomes/experience to change the status quo that has become the norm. Some of us even have backgrounds that include other skillsets your clinic might benefit from. Accounting, law, health management, and finance are just a few of my classmates former lives.
We are up to date with current evidence. Ask us! We know the clinical prediction rules based on the latest evidence. If you give us a shot, we may even be able to teach you a thing or two if you are willing to learn from us. Of course, we’re not expert clinicians, but current evidence and clinical expertise seems like a good marriage to me.
We seek outside mentorship. We all recognize that graduating from a great DPT program does NOT make us an expert. We also recognize that most clinics do not have the time to baby us and walk us through constant mentoring. The whole point of the DPT is so that a new grad could hit the ground running (if someone would hire us and give us the chance). Therefore, we see the importance of seeking independent mentorship outside of clinical hours.
We want to continue to learn and grow. With additional certifications, fellowships and residencies available, most of us want to continue to learn and earn specialty certifications. This in turn can help your clinic as we become more advanced. Engage us, and give us a pathway and you might be surprised where we end up.
We are moldable. You want to hire the perfect PT for your clinic. Hire a new grad and mold us into that perfect PT you desire! Where we lack in experience, we make up for in passion and excitement. We are open to criticism and suggestions of how we can be the best possible physical therapist.
We are the future of this profession. The PT field is growing rapidly and more and more students are applying to PT schools. That means the young PTs that are graduating were picked among tons and tons of applicants. We are a smart and utterly passionate group. WE deserve a fair shake in the applicant pool. If you find a new grad who is well spoken, involved, motivated, and a great fit for your clinic other than the lack of experience, I urge you to give them a shot. In a short while, they may become your best physical therapist.
If new grads are never given the opportunity to shine and grow, how are we as a profession going to move forward? I speak both personally and as the voice of many DPT students and new graduates- treat me like an asset and I will pour every ounce of passion and knowledge I have into becoming the best physical therapist for your clinic.
Links to Treating our Future Series Part 1: The Bane of the New Professional Part 2: New Grads, An Asset for Clinics Part 3: Resolving the Bane of the New ProfessionalTreating Our Future – Part 1: The Bane of the New Professional
As a professor in a few entry-level DPT programs over the past several years, I’ve had the privilege of getting to know many students. By and large, the graduates from these programs are some of the smartest, most motivated people I’ve met. However, they’re not always greeted with the same sentiment by employers. It’s concerning. It’s a situation worthy of not one, but several blog posts and so what follows is the first of a three-part series. I’ll start us off with this post to start a conversation about how the profession treats the people who are it’s future. In “New Grads: An Asset for Clinics,” Lauren Kealy, a DPT student at Regis University, gives a student perspective on why new grads are excellent assets in the clinic. In part three, we’ll look at some solutions, and incorporate feedback from the community as the conversation progresses.
Treating Our Future – Part 1: The Bane of the New Professional
My motivation for this blog post, and this series of posts, is not a good one. That said, I hope it sparks a constructive conversation that proves beneficial. Simply put, I’ve seen too many new professionals in physical therapy treated like dung by potential employers.
Here’s a story about how it goes for new grads here up in Colorado:
The new Grad looks for jobs. They don’t find many options, as the positions posted primarily request those with 3-5 years of experience. The newly minted doctor of physical therapy waits patiently for the ad accepting new grads. It never comes. They network, they reach out, they apply to jobs which request 3-5 years of experience anyway. Eventually, they get an interview, only to be told they don’t have enough experience. That’s even if they get a reply at all, as most often they get a polite thank you and never hear from the employer again.
After a while, they find a clinic who’s pressed to hire. Or they have a particularly strong networking connection. They then, to my personal dismay as an instructor, must perform a practical exam as part of the job interview to “test their hands.” I thought we already did that as part of their physical therapy education process? Was it not good enough? Didn’t the new graduate pass the NPTE? Is that not enough? Shouldn’t clinical reasoning be the thing you test instead of “hands,” especially if your clinic’s therapists use ultrasound regularly for patients with back pain? I don’t get it. But, let’s continue the saga of the job-seeking new graduate.
Provided they “pass” their practical exam, they are then sent on their way. If not hired, they still don’t often get a call back to let them know they weren’t hired. Silence is the most common answer. If hired, well, good for them. They’re on their way to greatness, albeit usually without benefits, or with minimal benefits and a salary that soon leads to sticker shock, as they contemplate the grizzly reality of paying off their 7 years of student loan debt and trying to afford a place to live.
At a recent #PTPubNight, I listened to a conversation between two clinicians. When one, the older, found out the person he was conversing with had less than 6 months of experience, he responded with a sneer, a statement, “Oh, you’re fresh!,” and a turn away from the previously strong conversation. Is this how we should be treating our profession’s future?
Dehumanizing our Future
It’s tragic to watch this process. From graduation and all of its ecstatic highs to the low of never even hearing “No,” new professionals in physical therapy can be in for a rough ride. It’s not that each new graduate deserves every job they apply for. However, they deserve the respect of a professional, qualified and ready to work. To not even return their application with a negative response, to question their skill set, to demean them for their lack of work experience is wrong, and unproductive. As the profession works to inspire leaders, innovators, and entrepreneurs to carry us into the future, a first stop characterized by disrespectful professional behavior is not a good strategy.
I know it’s not like this everywhere. In Texas, graduates from Texas State University were gobbled up like delicious pieces of bacon by clinics around the state. Texas is a positive job market, and so employers are happy to see the new graduates arrive. The point is, this happens somewhere. Colorado is not alone. I’ve conversed with many students from around the country and I hear similar themes: “They never even called me back, even after I did a hands-on practical.” “All the jobs want 5 years of experience, how am I supposed to get experience if no one will hire me?” “I had to sit and listen to what a liability I’d be for the clinic since I was a new grad.” “They made me do a practical exam, but the stuff they asked me seemed way out of date compared to what we learned in school.” I’ve spoken with many PT’s who declare, “I’ll never hire a new grad!” without remorse or pause. Many of these are the most respected and seemingly savvy PT’s around, even one’s with a large social media footprint.
It’s time for a conversation.
There are reason’s employers don’t want to hire a new graduate. Some of those are valid, while others are not. Some of the valid reasons, like lack of business skills or billing proficiency, should spark reform in education. Some of the invalid reasons, like assuming new grads can’t possibly manage patients with low back pain, should spark education and discussion. At no times, should the new professional be treated like dog meat as they rush excitedly into their first professional experiences. This issue is closely tied to the often discussed disconnect between education and clinical practice, but it’s more than that. It’s about respect, and a forward thinking strategy for how and where our new professionals go.
I’m very interested in feedback on this post. If you’re a clinic owner who doesn’t hire new grads, tell us why. If you’re a new professional, tell us about some of the hardships. If you just have an opinion, join in!
In part two of this series, Lauren will discuss the benefits of new professionals. Part three will look to solutions, and feature conversations that spawn from our posts, as well as highlighting some very successful practices who have embraced new graduates heavily. I look forward to this conversation.
Links to Treating our Future Series Part 1: The Bane of the New Professional Part 2: New Grads, An Asset for Clinics Part 3: Resolving the Bane of the New Professional#DPTSTUDENT CHAT TOPIC FOR WEDNESDAY, FEBRUARY 12, 2014: CSM 2014 WRAP UP! LIVE CHAT!
CSM was a week filled with exciting programming, buzzing nightlife, engaging conversation and invaluable new friendships. Probably the most exciting part for me was finally putting a face to a large portion of my twitter followers, professionals and the #DPTstudent’s we interact with on a daily basis!
While we hope to attend these conferences and experience all it has to offer, the reality is, unless you can be in three places at once you are probably missing out on something interesting. Each and every one of us has had a different experience at #CSM2014, so lets talk about it! The time is now to reflect upon what we have learned and how we will use this experience to promote our growth as a soon-to-be professionals. As we all settle back into normal everyday lives as #DPTstudent’s lets keep the CSM buzz going and reminisce on all the memorable experiences!
Join us this Wednesday at 9pm EST and tell us what you learned at CSM, what were some of your conference highlights and tell us why your experience at #CSM2014 was one to remember!
Blog post written by TJ Janicky (@TJ_Janicky)
#DPTSTUDENT CHAT TOPIC FOR WEDNESDAY, JANUARY 29, 2014: THRIVING AND SURVIVING #CSM2014
#CSM2014 is right around the corner and if not prepared, CSM can be quite an overwhelming experience for the novice conference goer. CSM has been compared to a marathon- an event that requires both mental and physical preparations but one that leaves the participant with an unforgettable adrenaline rush and a life altering sense of accomplishment. Consider this weeks #DPTstudent chat your last “long run” before the big race as we talk all about “Thriving and Surviving” at #CSM2014!
CSM is the LARGEST gathering of physical therapy professional and students and so it would only be fitting that this weeks #DPTstudent chat is the BIGGEST one yet. This week we will be bringing you, the #DPTstudent(s), a LIVE Google hangout and dual twitter tweetchat to capture what we hope will be the largest audience to date! Joining us for the LIVE Google hangout will be APTA Director and @APTASA BoD liaison Kathy Mairella (@KathyMairella), as well as Twitter guru and conference veteran Jerry Durham (@Jerry_DurhamPT). The chat will be full of helpful hints for program selection, time management, networking advice and tips for making the most of your time at #CSM2014!!
Be sure to keep an eye out for the link to the LIVE feed via twitter and the “Doctor of Physical Therapy Students” Facebook page, minutes before the chat at 9pm EST on Wednesday January 29th! Looking forward to what WILL be an amazing #CSM2014!!
Blog Post by TJ Janicky @TJ_Janicky). Chat hosted by TJ and Lauren (@laurenrSPT)
#DPTSTUDENT CHAT TOPIC FOR WEDNESDAY, JANUARY 22, 2014: APTA SECTION SPOTLIGHT: CARDIOPULMONARY PT!
The APTA Section Spotlight continues! This week we will be chatting with Richard Severin (@ptreviewer) who is a current resident at University of Wisconsin and a soon-to-be a Cardiopulmonary Certified Specialist…and the youngest one, at that! We will be talking to Richard about what cariopulm PT consists of, how he got involved in that specialty, and what opportunities being a section member brings. Talk to you on Wednesday at 9pm EST!
#DPTSTUDENT CHAT TOPIC FOR WEDNESDAY, JANUARY 15, 2014: APTA SECTION SPOTLIGHT- NEURO!
The APTA Section Spotlight continues this week featuring the Neurology section! We will be joined by some section members and neuro PTs that help treat everything from traumatic brain injuries to patients recovering from stroke. Please join us this Wednesday at 9pm EST to learn about benefits of being a student member in the neuro section, mentorship opportunities, and to connect with some of the best neuro PTs on Twitter!
Follow the APTA Neurology section on Twitter at @APTA_NeuroPT and check out their website here!
#DPTSTUDENT CHAT FOR WEDNESDAY, JANUARY 8TH, 2014: APTA SECTION SPOTLIGHT: ACUTE CARE
Happy New Year #DPTstudent(s) and welcome back! We are excited to kick off the new year of the #DPTstudent chat by continuing our “Section Spotlight” with the APTA Acute Care Section (@acutecarept)!
Acute care physical therapy encompasses a wide range of clinical settings including hospitals, skilled nursing units, sub-acute rehabilitation centers, home care, and acute rehabilitation centers. Acute care physical therapy is unique in that the patient population is “acutely ill” with an active disease process or trauma, while also working through a decrease in physical function. Among many other skills, acute care physical therapists must be equipped with a solid understanding of post op movement contraindications, lab values and modern monitoring devices including the various intravenous lines and monitors. The acute care setting is often fast paced and requires the therapist be able to think quickly in the case of an emergency.
We are extremely excited to have the APTA Acute Care Section joining us this Wednesday, January 8th at 9pm EST, to discuss all things acute care as well as student benefits of being an acute care section member! For more information on APTA’s Acute Care section please visit www.acutpt.org and check out some of the student opportunities under the “students” tab!
Blog post written by TJ Janicky (@TJ_Janicky).
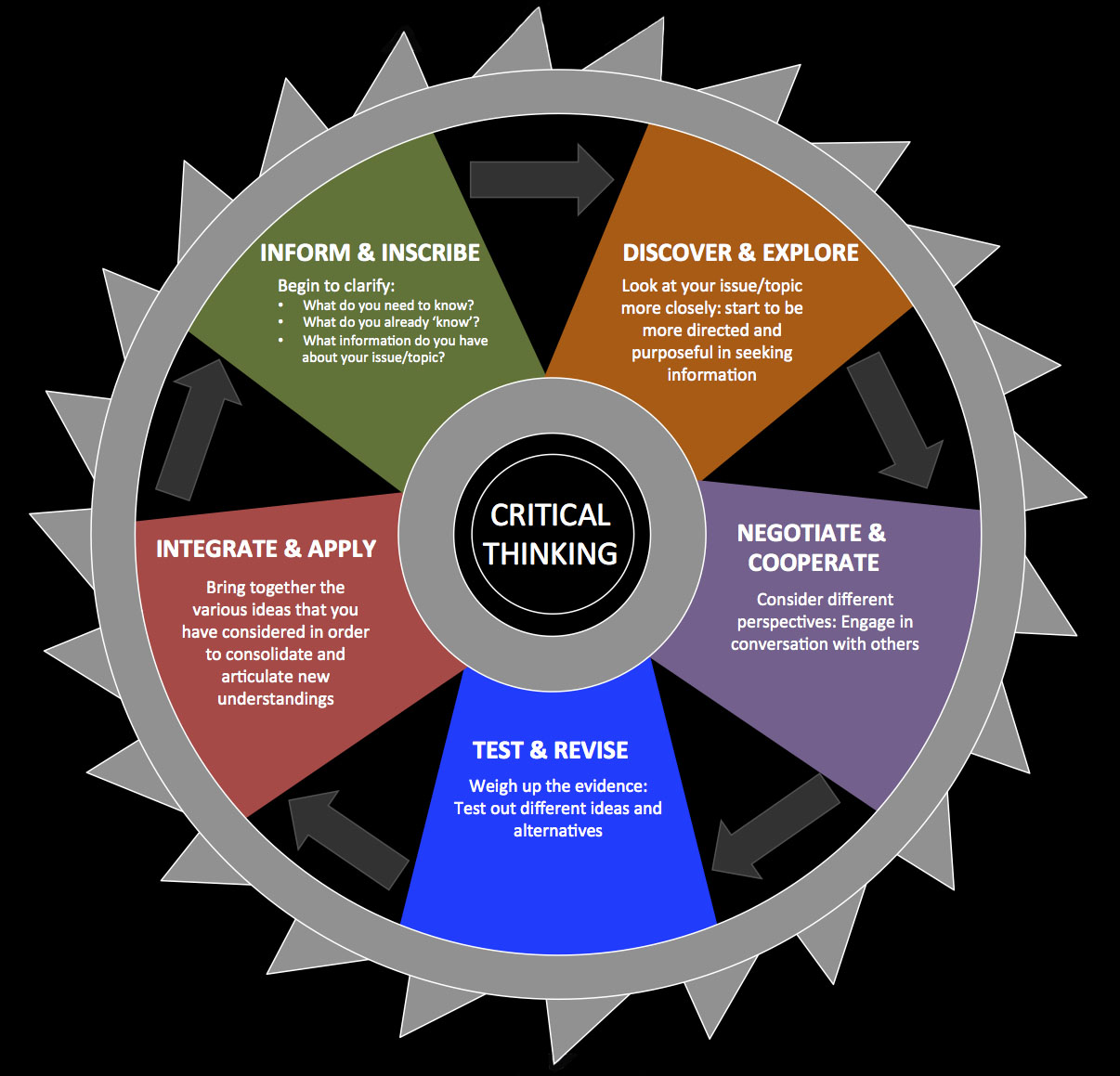
Metacognition, Critical Thinking, and Science Based Practice #DPTstudent
Metacognition can be considered a synonym for reflection in applied learning theory. However, metacognition is a very complex phenomenon. It refers to the cognitive control and monitoring of all sorts of cognitive processes like perception, action, memory, reasoning or emoting.
A recent #DPTstudent tweet chat dealt with the concept of metacognition broadly (list of links), but more specifically discussed the need for critical thinking in education and clinical practice. Most agreed on the dire need for critical thinking skills. But, many #DPTstudents felt they had no conceptual construct on how to develop, assess, and continually evolve thinking skills in a formal, structured manner. Many tweeted they had never been exposed to the concept of metacognition nor the specifics of critical thinking. Although, most stated that “critical thinking” and “clinical decision making” were commonly referenced.
What’s more important than improving mental skill sets?
Thinking is the foundation of conscious analysis. Yet, even with a keen focus on assessing and improving our thinking capacities, unconscious processes influence not only how and why we think, but what decisions we make, both in and out of the clinic. We are humans. Humans with bias minds. Brains that, by default, rationalize not think rationally…
Everyone thinks; it is our nature to do so. But much of our thinking, left to itself, is biased, distorted, partial, uninformed or down-right prejudiced. Yet the quality of our life and that of what we produce, make, or build depends precisely on the quality of our thought. Shoddy thinking is costly, both in money and in quality of life. Excellence in thought, however, must be systematically cultivated. – Via CriticalThinking.org
Need a Model
Mary Derrick observed previously in her post that the words critical thinking and clinical decision making are often referenced without much deeper discussion as to what these two concepts entail or how to develop them. Students agree that critical thinking and sound clinical decision making are stressed in their pre-professional education. But, all levels of education appear to grossly lack formalized courses and structured approaches. The words are presented, but rarely systematically defined. The actual skills rarely practiced and subsequently refined. Students thus lack not only exposure and didactic knowledge of metacognition, critical thinking, and decision making, but also lack experience evolving these mental skills.
Need to teach how to think
Alan Besselink argued a scientific inquiry model to patient care is, from his view, “the one approach.”
There is, in fact, one approach that provides a foundation for ALL treatment approaches: sound, science-based clinical reasoning and principles of assessment, combined with some sound logic and critical thinking.
One approach to all patients requires an ability to gather relevant information given the context of the patient scenario. This occurs via the clinician’s ability to ask the appropriate questions utilizing appropriate communication strategies. Sound critical thinking requires the clinician to hold their own reasoning processes to scrutiny in an attempt to minimize confirmation bias if at all possible. It also requires the clinician to have a firm regard for the nature of “normal” and the statistical variations that occur while adapting to the demands of life on planet earth.
Philosophically, I agree. It appears the question “what works?” has been over emphasized at the potential sacrifice of questions such as “how does this work?” “why do we this?” and “why do we think this?”
Unfortunately, the construct of evidence based practice assumes the user applying the EBP model is well versed in not only research appraisal, but critical thinking. The structure of evidence based practice overly relies on outcomes studies. It lacks a built in process for integration of other sources of knowledge as well as the applicable question of “does this work as theoretical proposed?” The evidence hierarchy is structured and concerned with efficacy and effectiveness only. Many will be quick to point out that from a scientific rigor standpoint the evidence hierarchy is structured as such, because other forms of inquiry (basic physiology, animal models, case reports, case series, cohort studies, etc) can not truly answer questions “what works?” without significant bias. Robust conclusions on causation can not be made via less controlled experiments. And this, of course, is true. In terms of assessing effectiveness and efficacy in isolation, the evidence hierarchy is appropriately structured.
But, the evidence hierarchy does not consider knowledge from other fields nor basic science, and thus by structure explicitly ignores plausibility in both theory and practice. To be fair, plausibility does not necessarily support efficacy nor effectiveness. So, it is still imperative, and absolutely necessary, to learn the methodology of clinical science. Understanding how the design of investigations affects the questions they can truly answer precedes appropriate assessment and conclusion. Limits to the conclusions that can be drawn are thus explicitly addressed.
Need the Why
Because of the focus on evidence based practice, which inherently (overly?) values randomized control trials and outcomes studies over basic science knowledge and prior plausibility, students continue to learn interventions and techniques while routinely asking “what works?” Questions of “how did I decide what works?” “why do I think this works” and “what else could explain this effect?” also need to be commonly addressed in the classroom, clinic, and research. Such questions require formalized critical thought processes and skills.
These questions are especially applicable to the profession of physical therapy as many of the interventions have questionable, or at least variable, theoretical mechanistic basis in conjunction with broad ranging explanatory models. This is true regardless of effectiveness or efficacy. In fact, it is a separate issue. Physical therapy practice is prone to the observation of effect followed by a theoretical construct (story) that attempts to explain the effect. A focus on outcomes based research perpetuates these theoretical constructs even if the plausibility of the explanatory model is unlikely. In short, while our interventions may work, on the whole we are not quite sure why. @JasonSilvernail‘s post EBP, Deep Models, and Scientific Reasoning is a must read on this topic.
The profession suffers from confirmation bias in regards to the constructs guiding the understanding of intervention effects. In addition, most, if not all, interventions physical therapists utilize will have a variety of non-specific effects. These two issues alone highlight the need for critical thought in order to ensure that our theoretical models, guiding constructs, and clinical processes evolve appropriately. And, further, to facilitate appropriate interpretation of outcomes studies.
It is not “what works?” vs. “why does this work?” Instead, a focus on integrating outcomes studies into the knowledge and research of why and how certain interventions may yield results is needed. This requires broadening our “evidence” lens to include physiology, neuroscience, and psychology as foundational constructs in education and clinical care. Further, research agendas focused on mechanistic based investigations are important to evolving our explanatory models. Education, research, and ultimately clinical care require both approaches. Interpretation, integration, and application of research findings, be they outcomes or mechanistic, necessitates robust cognitive skills. But, do we formally teach these concepts? Do we formally practice the mental skills?
So, now what?
There appears to be an obvious need, and obvious value, to learning how to think. But, that is just the start. The necessity of learning to think about thinking is required to improve the specific skill of critical thinking. The understanding and application of evidence based practice needs more robust analysis. Growth of critical thinking, metacognition, and an evolution of evidenced based to science based practice produces the foundation for strong clinical decision making. The call for evidence based medicine to evolve to science based medicine focuses on ensuring clinicians interpret outcomes studies more completely. It appears to put strong emphasis on increased critical thinking and knowledge integration.
Does Evidence Based Medicine undervalue basic science and over value Randomized Control Trials?
A difference between Sackett’s definition [Evidence Based Practice] and ours [Science Based Medicine] is that by “current best evidence” Sackett means the results of RCTs…A related issue is the definition of “science.” In common use the word has at least three, distinct meanings:
1. The scientific pursuit, including the collective institutions and individuals who “do” science;
2. The scientific method;
3. The body of knowledge that has emerged from that pursuit and method (I’ve called this “established knowledge”; Dr. Gorski has called it “settled science”).
I will argue that when EBM practitioners use the word “science,” they are overwhelmingly referring to a small subset of the second definition: RCTs conceived and interpreted by frequentist statistics. We at SBM use “science” to mean both definitions 2 and 3, as the phrase “cumulative scientific knowledge from all relevant disciplines” should make clear (by jennifer). That is the important distinction between SBM and EBM. “Settled science” refutes many highly implausible medical claims—that’s why they can be judged highly implausible. EBM, as we’ve shown and will show again here, mostly fails to acknowledge this fact.
What to do?
1. Learn how humans think by default: Biased
2. Learn the common tricks and shortcuts our minds make and take
3. Understand logical fallacies, cognitive biases, and the mechanics of disagreement
4. Meta-cognate: Think about your own thinking with new knowledge
5. Find a mentor or partner to critique your thought processes: Prove yourself wrong
6. Critique thought processes, lines of reasoning, and arguments formally and informally
7. Debate and discuss using a formalized structure
8. Think, reflect, question, and assess
9. Discuss & Disagree
10. Repeat
Science Based Practice…
1. Foundations in basic science: chemistry, physics, physiology, mathematics
2. Prior plausibility: “grand claims require grand evidence”
3. Research from other relevant disciplines from physics to psychology
4. Mechanics of science: research design and statistics
5. Evidence Based (outcomes) Hierarchy
Questions lead, naturally, to more questions. Inquiry breads more inquiry. Disagreement forms the foundation of debate. And thus, Eric Robertson advocates for embracing ignorance
Ignorance is not an end point. It’s not a static state. Ignorance isn’t permanent. Instead it’s the tool that enables one to learn. Ignorance is the spark that ignites scholarly inquiry.
Ignorance: the secret weapon of the expert.
Growth is rarely comfortable, but it’s necessary. And, that’s a lot to think about….
Resources
A Practical Guide to Critical Thinking
CriticalThinking.org
Logical Fallacies
Critical Thinking Structure
List of Fallacies
List of Cognitive Biases
Science Based Medicine
Clinical Decision Making Research (via Scott Morrison)
Clinical Decision Making Model
Thinking about Thinking: Metacognition Stanford University School of Education
Occam’s Razor
The PT Podcast: Science Series
Understanding Science via Tony Ingram of BBoyScience
I don’t get paid enough to think this hard by @RogerKerry1 (his blog is fantastic)


