[list][/list]Sometimes, it’s pure and simple logic that prevails as the best solution to something. This was the case in an important new study published ahead of print in Spine. You may have seen the presser released by APTA, AAOMPT on the matter. They’re exuberant, and they should be. Well, mostly.
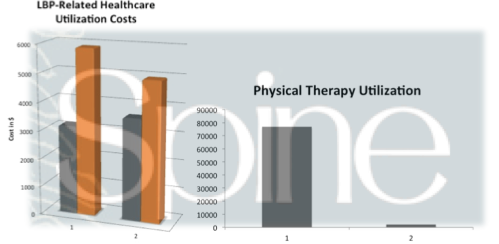
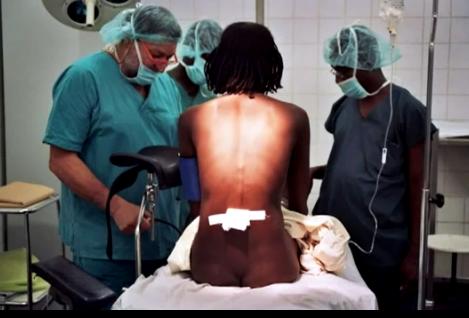
The study, published by Drs. Julie Fritz, John Childs, Rob Wainner, and Tim Flynn, examined a payor database and looked at over 32,000 data sets of patients with low back pain with the purpose of describing physical therapy utilization in primary care settings. Further, they looked at both associated healthcare costs and the question of whether the physical therapy care being provided was either adherent with practice guidelines for an active treatment or non-adherent. Treatments were classified as non-adherent when they included things like ultrasound that are not proven interventions for patients with low back pain. While not a perfect practice, the researchers used billing codes as their determination factor for treatment adherence.
The findings of this study are fascinating to me. Albeit, many public health studies that look at low back pain and care patterns and/or costs are fascinating to me, so I’ll let you be the judge.
The key findings of the study were:
[list style=”circle”]
- For patients receiving physical therapy, early referral (within 14 days) was associated with less overall healthcare utilization, which included lower use of surgery, fewer doctor visits, less injections, and less advanced imaging that those with delayed referral (14-90 days).
- For patients receiving adherent care, overall health utilization was also lower, but to a lesser degree that that seen with the early referral group.
[/list]
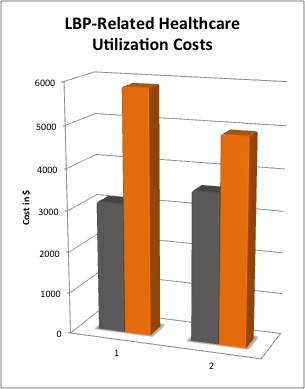
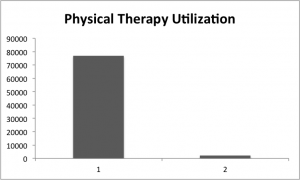
As you can see by the graph above, significant savings were realized by early referral to physical therapy and by adherent physical therapy care. Logic sure does shine forth here. If you’re going to go somewhere, well you might as well just get there. Significantly, the finding in this study is important because it runs counter to the suggestions by many LBP practice guidelines that suggest primary care physicians delay referral to other services as many patients are likely to improve anyway. Overall trends to reduce the medicalization of LBP are important, but this study reflects a trend whereby physicians are referring about half of patients to physical therapy within 14 days anyway. It turns out, this may end up being an evidence-supported practice.
Not all was rosy, however. Here are some other findings that were important:
[list style=”circle”]
- Overall utilization for physical therapy for patients with low back pain in this data set was only 7%.
- Overall healthcare costs were higher for patients receiving physical therapy. This might reflect increased severity, co-morbidities, etc, we just don’t know.
- Only 21% of the physical therapy care provided was able to be classified as adherent. This could reflect an imperfect measuring tool, but I suspect there’s a problem here.
- Wide geographic variability persists in the management of LBP, including physical therapy utilization and adherence to guidelines.
[/list]
This study is full of many other gems. It’s gated at Spine, so apologies for not including a full text link. The good new: Spine is a huge journal and this will be seen. As with many studies, this leaves more questions to ask. Such as, what factors make the patients who are referred early have lower subsequent utilization. The authors hypothesize it may have to do with the concept of self-efficacy. I like it.
I like it so much, in fact, that I’m involed in a related study with some of the authors to examine a similar question in a Department of Defense database. I’m eager to see what we find.
This study was jointly funded by grants from the Orthopaedic and Private Practice sections of the APTA, AAOMPT, and a faculty research grant from Texas State University.