Mary McMillan is a founder and the first president of the American Physical Therapy Association. She wasn’t the first person to practice physical therapy, but as Mildred Elson stated in her 1964 McMillan lecture, “She thought in terms of the whole country and foresaw its great civilian need for physical therapy.”
She’s also a bad ass.
Here’s her story, in memes.
Note: The majority of this re-telling of Mary McMillan’s history has been pulled from her speech in 1946, entitled “Physical Therapy from the Embryo on Three Continents,” and the 1944 annual conference proceedings at which Mary McMillan was awarded an honorary active lifetime membership in the APTA. The proceedings were published in Physiotherapy Review, now the Physical Therapy Journal.
Mary McMillan was raised in England and completed her studies at the University of Liverpool Gymnasium, where they were offering a 2 year course in physical education. She also took a break from these studies to head to London for further courses in neuroanatomy, neurology, and psychology.
1.
At the outbreak of World War I, Mary applied for a Voluntary Aid Detachment (VAD) unit out of the University of Liverpool. Fortunately for physical therapy in the United States, she failed the medical examination and decided to travel to Boston…during the war, in a convoy, under complete blackout conditions.
After arriving in the US, she met Marguerite Sanderson, another important figure in the development of physical therapy. She was put to work at Walter Reed Hospital, and matter-of-factly states: “That was the beginning of physical therapy in the US Army.” Physical therapy was accorded as a health service in 1917 by the US Army.
Mic drop.
2. 
Dr. Everett Beach, from Reed College in Portland Oregon, wanted Mary to come teach the 200 potential reconstruction aides (the original name for physical therapists) he had signed up for an emergency course to assist with the war effort. Mary immediately applied for a leave of absence from the Army to go where she was needed. When the Army dragged its feet, she threatened to resign. Within 24 hours, she was granted a leave of absence, and left for Portland.
So that’s how that’s done.
3. 
Post WWI, a letter was sent to the reconstruction aides, asking if they wanted to see a professional association built. The answer was a resounding yes. Here are some cool facts about what they built, from Eleanor Carlin’s 1976 McMillan Lecture:
- “Whether by design or accident…nothing was said about working only under the direction of a physician” (Carlin, p. 1113).
- Our founders had the foresight to include policy that would allow the development of chapters, and they almost simultaneously founded the Physical Therapy Journal, ensuring that publication was valued.
- The Association was originally called the American Women’s Therapeutic Association, but charter members realized that this would be alienating to men, and voted to change the name to the American Physiotherapy Association. The first man was elected to national office in 1942.
- Women entering the profession were required to have a college education.
- By 1924 the charter members had discussed the standardization of physical therapy through state registration and licensure. By 1971, practice acts had been established in all 50 states (Blair, 1971).
4. 
Mildred Elson, first McMillan Lecturer, first president of the World Confederation of Physical Therapy, and first president of the Wisconsin Physical Therapy Association, quotes Mary McMillan: “What we need is one unanimous effort in order to establish a high standard for our profession and enthusiasm that knows no bounds.”
Elson goes on to say in her 1964 lecture, “Early members at the first convention did not join & say, “What can I get out of it,” they said, “I intend to join to see what I can make out of my profession and to see what I can do to create and maintain standards.” So on that note, you know the APTA is trying to reach 100k members, right? Check it out here.
5. 
After WWI, Mary answered the call from the China Medical Board of the Rockefeller Foundation to work in the Peking Union Medical College in China. Of course, the Rockefeller Foundation knew who she was, and Mary took charge of the Department of Physical Therapy at Peiping Union Medical College in 1932. She first got rid of the “obsolete apparatus” in the gymnasium, then set about finding people who were up to her standards. In her speech, “Physical Therapy from the Embryo on Three Continents,” she states: “This necessitated that some people must be taken off the payroll—it was not an easy thing to do—it hurt me very much to do it, but it had to be done. I was able to replace these people with more modernly trained nurses and a physical education graduate.”
She also set up scholarships to encourage graduates to apply, and partnered with a physician to head the department.
6. 
November 1, 1941, all Americans were urged to evacuate Peking. Mary, along with several others, wound up in Manila (capital of the Philippines) in a roundabout way to get home, with no chance of sailing before December 20. December 7, 1941, Pearl Harbor was bombed. Mary offered her services to the Army Hospital in Manila, where she was one of the first to assist the dead and wounded upon arrival. Christmas Eve, Manila fell to the Japanese. Mary, realizing what was about to happen, “borrowed” a truck, and with 3 women drove to the hospital to recover drugs, instruments, beds, and bedding. These supplies furnished the internment camp hospital at Santa Tomas. Mary slept on a filing cabinet.
7. 
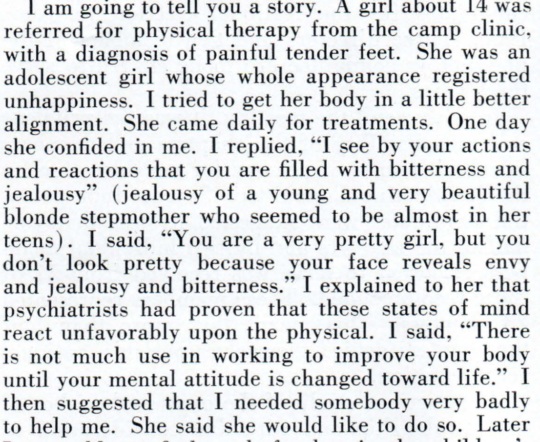
Mary, who referred to her work in the Japanese internment camps as her “swan song” recalled this episode of patient care:
8. 
Mary McMillan was repatriated in 1943. When she stepped off the boat, she was met by Dorothea Beck, previous editor of the Physical Therapy Review. She continued to be a source of strength and inspiration to the Association until her death in 1959. She assisted with efforts to found the World Confederation of Physical Therapy and was known to show up at parties. Margaret Moore, the 1978 McMillan Lecturer, recalled: “…a lively party with lots of people, loud music, much dancing, and rattling of glasses was taking place at my home. Who should appear at my front door but Molly McMillan…Within 10 minutes, Miss McMillan was in the middle of the group with her shoes off…I treasure the moments with that fun-loving, warm, and lovely lady.”
References
Blair, Lucy. “Past Experiences Project Future Responsibilities.” Physical Therapy 52.5 (1971): 493-99. Print.
Carlin, Eleanor J. “The Revolutionary Spirit.” Physical Therapy 56.10 (1976): 1110-116. Print.
Elson, Mildred, ed. “Twenty Third Annual Conference.” The Physiotherapy Review 24.4 (1944): 148-50. Print.
Elson, Mildred O. “The Legacy of Mary McMillan.” The Journal of the American Physical Therapy Association 44.12 (1964): 1066-072. Print.
McMillan, Mary. “Physical Therapy on Three Continents.” The Physical Therapy Review 40.2 (1960): 140-43. Print.