A recent article entitled “Why industry surveys on physician adoption of smart phones could be overestimating reality”at iMedicalApps [Mobile Medical App Reviews & Commentary – A publication by medical professionals] explored what recent market research really means…
It has been cited in market research that 72% to 94% of physicians are using smart phones in clinical practice (Questions: How are they using them? And, how often?). Josh Herigon, MPH a second year medical student and blogger at Number Needed to Treat comments:
“Although these studies show a high degree of smartphone adoption among physicians, these results should be interpreted cautiously. These firms provide few details on how they actually conducted these studies. A major hurdle to conducting such research is sampling bias. This can occur in survey research when researchers get a low response rate (i.e.—researchers approach a large number of individuals to fill out a survey but few actually fill it out).”
A little bird told me that a PTJ internal study revealed that no more than 50% of the physical therapists they sampled used smart phones. And, while the percentage of professionals who have and use smart phones is interesting data, I think there is a bigger question to consider. How many physicians, physical therapists, and other healthcare providers who own smart phones are using them routinely and effectively in clinical practice?
Owning a smart phone and leveraging its capabilities during clinical practice are two vastly different things. I am an avid smart phone owner and user, but to be honest, I rarely use my phone in clinical practice. I actually use it most while practicing within the in-patient hospital setting to look up medications, abbreviations, surgeries, and specific diagnoses. But, that is only when I am not near, or logged into, a computer. Admittedly, in the outpatient setting I grossly underuse the capabilities of my phone.
Why are we still giving out paper copies of exercises and patient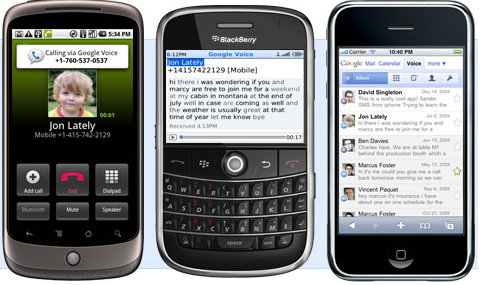 education? I believe the opportunities for leveraging this technology for clinical support, aiding in clinical decision making, and pt. education are infinite. In my opinion, routine use could actually markedly increase efficiency and quality of care especially in physical therapy. Patient’s use and love their smart phone, so why aren’t we interfacing with them using technology? [Yes, I understand the potential HIPPA considerations and that is not the point of this post]
education? I believe the opportunities for leveraging this technology for clinical support, aiding in clinical decision making, and pt. education are infinite. In my opinion, routine use could actually markedly increase efficiency and quality of care especially in physical therapy. Patient’s use and love their smart phone, so why aren’t we interfacing with them using technology? [Yes, I understand the potential HIPPA considerations and that is not the point of this post]
- Patient education
- Home exercise programs: Pictures, videos, directions
- Pictures and videos of patient performance (motor control, motor learning, and feedback)
- Documentation
- Scheduling
Do you think it would be possible to run a private practice and physical therapy LLC strictly from a smart phone. If not, why not? Paper is messy and overated anyway…
Do you have a smart phone? If so, how are you using your smart phone in clinical practice? Do you use specific applications? Any ideas for how we can better utilize this technology as we move forward?
Considering making the switch to a smart phone? Check out this article targeted towards medical professionals: iPhone, Blackberry, or Android?



 The other issues we face when evaluating the iPad as a medical tool are fragility (it will break if dropped) and hygiene since it cannot be sterilized. The latter is probably less of an issue for physical therapists than other medical professionals, but certainly bears mentioning.
The other issues we face when evaluating the iPad as a medical tool are fragility (it will break if dropped) and hygiene since it cannot be sterilized. The latter is probably less of an issue for physical therapists than other medical professionals, but certainly bears mentioning.