Having just defended a dissertation in the field of neuroscience, this session was my guilty pleasure. I felt right at home hearing about the modulation of intrinsic motor neuron properties. But, the question I’ve had since graduate school was the focus of this session – how does the lab work in cat/rat/monkey motor neurons translate to human patients?
This session was presented by four brilliant researchers interested in brainstem modulation of the motor system. The patient population discussed was spinal cord injury, a condition in which the connection between the brainstem and the motor neurons are disrupted. Each researcher discussed the implications for force generation, spasticity, and locomotion. I’ll summarize their reports below.

Allison Hyngstrom, PT, PhD
First up, Dr. Hyngstrom highlighted a few key researchers that have influenced treatment of patients:
- Sherrington – contributed the concept of the spinal motor neuron as the final common pathway – contributed to the understanding of locomotion by examining “air stepping” elicited by stretching hip muscles of spinalized
- Eccles – introduced the idea that inhibition could sculpt the output of motor neurons, particularly the reciprocal inhibition pathway
- Brown/Grillner/Lundberg – descending input, as well as specific neurotransmitters, could activate spinal networks without sensory inputs
The Dr. Hyngstrom progressed to ‘Motor Neurons 101’, including these key points:
- MNs possess huge denritic trees to receive inputs from several sources (higher brain, local interneurons, afferent)
- Two categories of receptors are expressed on the MN membrane – ionotropic and metabotropic
- The activation of metabotropic receptors by monoamines create persistent inward currents (PICs)
- PICs can amplify the output of the MN
- In acute spinal cord injury there is a loss of seratonin in the spinal cord that decreases the excitability of spinal MNs
Moving to the spinal cord injured cat, researchers have found that by adding monoamines to the spinal cord the cat could walk again [link to article in PubMed]
Next Dr. Hyngstrom described some of her own work on MNs. In her dissertation she was interested in the factors that regulate PICs. One way she did this was by altering the amount of reciprocal inhibition.
In summary
- Monoamines (like seratonin) increase the gain of the MN > which implies PTs could reduce effort for a given movement
- Monoamines facilitate automatic movements
- Dysregulation of monoamines likely contributes to alterations in cellular excitability in chronic spinal cord injury
- Altered cellular excitability not necessarily a bad thing > consider other ideas
- Targeted medications could be used to harness spinal network excitability
Chris Thompson, PT, DPT
Next up Dr. Thompson presented his talk, titled – “Activation of spinal networks in patients with spinal cord injury to improve volitional movements”.
He began with a bold statement – “indiviuals with motor incomplete SCI do not fatigue”. How could this be? It seems that in a repeated stimulation protocol, patients with acute SCI do not exhibit a reduction in force generating capacity, whereas patients with chronic SCI and healthy controls do exhibit a reduction in the same protocol.
I also seems that people with incomplete SCI have a reserve of volitional force generation – 115% of maximal force can be achieved across the first 4-5 maximal contractions.
In acute spinal cord injury there is a period of spinal shock and spinal reflex responses are suppressed. But after time (chronic) the responses become super sensitive to seratonin.
Dr. Thompson want to know why and he looks to the motor neuron persistent inward current as a mechanism for the following three reasons:
- There is an increased EMG amplitude across contractions, through increased recruitment and rate modulation of motor units
- Prolonged torque in response to electricla stimulation using top hat stim protocol, which was abolished when a nerve block was in place
- There are alterations in motor unit activity due to pharmacological agents (SSRI), which block the reuptake of seratonin
Dr. Thompson concluded by review attempts at translation of the findings in animal models to humans patients. The idea best examined by his lab group basically involves applying a ‘top-hat’ stimulation protocol made popular in cat experiments to human patients. Something very interesting happens when comparing humans and cats. The amount of force and the strength of the persistent inward current are larger when muscles are at shorter lengths IN HUMANS. However, the amount of force and the strength of the PIC are larger when muscles are at longer lengths IN CATS. Explaining this difference is the next task on Dr. Thompson’s plate.
 Arun Jayaraman, PT, PhD
Arun Jayaraman, PT, PhD
Alright, that was a lot of motor neuron physiology and I appreciate you hanging in there so far. So, how can the above information be put into clinical practice? This is what Arun enthusiastically addressed – developing the rehabilitation protocol.
His main question was how can we harness the reserve in force generating capacity seen in patients with incomplete spinal cord injury?
This was tested in 10 patients with chronic motor incomplete SCI in a cross-over design with a two month washout period between the testing conditions. The phenomenon examined was that the harder you work, the more force enhancement you observe in the SCI population. As the time between maximal contractions gets longer, the enhancement in force production becomes lower (15 s is best). This phenomenon is present both concentric and isokinetic contraction modes.
Subjects trained with 65-80% of their one repetition maximum until they plateaued in function. Arun found that just isometric trained alone enhanced berg balance scores and walking distances in the 6-min and timed up and go tasks. Noxious stimulation at an intensity of 50 mA on the stomach skin was not so effective.
A follow up direction Arun is investigating is the use of intermittent hypoxia. It has been shown in rats that electromyography and force measurement improved in a ladder climbing task following a hypoxic state. How will patients with chronic SCI respond to hypoxic conditions during locomotor training? Arun is hopeful that benefits are realized in his patients.
In summary
- Volitional drive can be enhance by working very hard
- Does improve walking and balance
- Can be done at home
- What are long term effects?
- Can this be complimented with intermittent hypoxia?
 George Hornby, PT, PhD
George Hornby, PT, PhD
The topic addressed by Dr. Hornby at the end of the session was the combination of physical therapy and pharmacological interventions.
It seems that providing glutamate can generate locomotion patterns and we also know that monoamines can excite central pattern generators (CPGs).
There is an increased Babinski Sign in SCI due to effects of monamines.
Seratonin (5HT) is effective in initiating locomotion in rats with SCI.
It seems that humans respond better to 5HT than norepinephrine (NE) when administered.
Lastly, Dr. Hornby has seen that strength, not spasticity, is related to locomotion function.
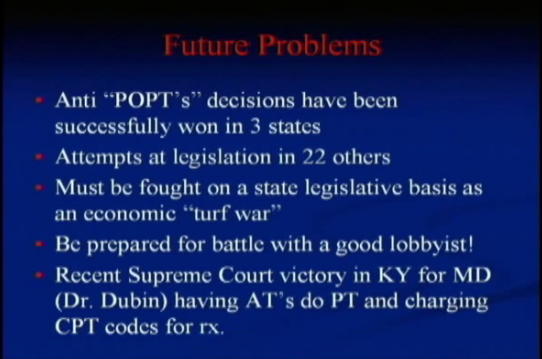
 Luckily, NBC LA continues to provide top notch coverage and analysis of the issues in their THIRD article entitled Caution: State Laws Hazardous to Your Health. In the comments section Johnny Chen makes a great point:
Luckily, NBC LA continues to provide top notch coverage and analysis of the issues in their THIRD article entitled Caution: State Laws Hazardous to Your Health. In the comments section Johnny Chen makes a great point: