Succès de scandale!
Well, physical therapy didn’t exactly have a sex tape this week, but over the past several days, two notably large media outlets have featured PT in ways we might not, at first glance, like to be defined. The most prominent of these was physical therapist, Peggy Brill, who appeared on the Dr. Oz show to tout Ultrasound, Tiger Balm patches, and Bumpy Balls as cutting edge treatments for back pain.
 The second piece may have been slightly smaller in reach, but not if you’re a regular internet news surfer. An article that originated on the website, Greatist.com, made its way to media juggernaut, The Huffington Post. The article, entitled, “The 8 Best Physical Therapy Methods Explained,” featured “Greatist Experts Dr. Mike Reinold and Dr. Eugene Babenko.” The troubling part about these spots, which drew national attention, is that of the 11 treatments extolled by the PT’s, only 2 were not weakly supported passive modalities. When you take a step back and look at the brand message being delivered, it says ‘Physical Therapy consists of ultrasound, electric stimulation, lasers, traction, heat, ice, smelly patches, something that resembles children’s toys, and oh, exercise and something called manual therapy. Yes, I cringe.
The second piece may have been slightly smaller in reach, but not if you’re a regular internet news surfer. An article that originated on the website, Greatist.com, made its way to media juggernaut, The Huffington Post. The article, entitled, “The 8 Best Physical Therapy Methods Explained,” featured “Greatist Experts Dr. Mike Reinold and Dr. Eugene Babenko.” The troubling part about these spots, which drew national attention, is that of the 11 treatments extolled by the PT’s, only 2 were not weakly supported passive modalities. When you take a step back and look at the brand message being delivered, it says ‘Physical Therapy consists of ultrasound, electric stimulation, lasers, traction, heat, ice, smelly patches, something that resembles children’s toys, and oh, exercise and something called manual therapy. Yes, I cringe.
Now, before you hire the lynch mobs to go find these blasphemous physical therapists who soured the public’s view of the profession, pause for a moment and understand how the media works. PT’s do not direct and produce media development. Often, by the time the expert is contacted, the direction of a particular spot is already formed. I will say the Brill Dr. Oz video is difficult to defend, but if you look closer at the Greatist.com article, you’ll see that Mike Reinold did try his best to steer the article.
Statements like, “Ultrasound has also been shown to increase ligament-healing speed in our furry counterparts (read: rats), though more studies are needed to show whether the same holds true for us,” and “Note: Heat is just one tool to help the therapist be more effective, Reinold says, it shouldn’t be the main focus of a treatment plan,” clearly show how Dr. Reinold was trying to steer the article and minimize the message of passive modalities. He even tweeted later on that the author did a great job of taking his feedback on the article. I know Mike well and he’s not a slayer of physical therapy. He’s an advocate, and a powerful one at that, with a large audience who follows his rehab, sports medicine, and performance blog, MikeReinold.com. Still, the average internet reader and skimmer probably saw, Best PT = Ice, Heat, Ultrasound, Traction, etc. Yes, the article started with Manual Therapy being listed, but I argue that most readers wouldn’t recall that in their skimming compared to the more easily imaged words familiar to them, like heat and ice.
I can relate to this idea of physical therapy by mainstream media. I was interviewed recently for an article being prepared for a national publication. I spent most of the time in the interview trying to convince the writer that their preconceived notions of physical therapy weren’t actually physical therapy. I was moderately, but not fully successful. At a certain point, I had to draw the line or risk the writer moving on to a different “expert” who may have been more passive than I. And that’s the reality of media development. We should accept that the public has a very modality-based view of us and think of strategies to fix this.
Physical Therapist philosophizer, Allan Besselink, responded to the Greatist article, expressing not only his distaste for yet another passive treatment article, but also his idea of the 4 best physical therapy treatments for patient-centered care. He writes,
Here are the four best physical therapy methods for patient-centered care:
1. Mechanical assessment: The best treatment will be a natural progression from a good mechanical assessment based on sound clinical reasoning strategies.
2. Patient education: The patient needs to understand the solutions to their problem, the self care strategies involved, and the self-monitoring and progression of these strategies.
3. Exercise: Patient- and condition-specific exercise programs are critical self care strategies to promote optimal repair and remodeling, along with effective reduction of mechanical derangement if present. Exercise should be evidence-based and supported by the sport sciences research.
4. Mentorship and guidance: Physical therapists have the knowledge base and capacity to act as health mentors, providing instruction, progression, and guidance as necessary.
Of course, none of these sound quite so fancy or high-tech as laser or ultrasound. But they all depend on the consumer’s active involvement in their care. Isn’t that the message we really want to send to consumers?
Allan’s list is excellent, though I would change out the first item for something more recognizable to the patients. The Doctors of Physical Therapy blog developed a similar list. Perhaps my reworked list might look like this:
Eric Robertson’s List of the 5 Best Physical Therapy Treatments for Patient-Centered Care: (stealing some parts directly from Alan)
1. Mentorship and Guidance: Physical therapists have the knowledge base and capacity to act as health mentors, providing instruction, progression, and guidance as necessary. Inherent in this is the fact that physical therapy treatment is continually distilled with excellent patient education about their condition and road to health.
2. Exercise: Exercise is the super power of the human physiology. Patient- and condition-specific exercise programs are critical self care strategies to promote optimal repair and remodeling of all your body’s systems. Exercise should be evidence-based and supported by the sport sciences research.
3. Pain Reduction: Through an integrated strategy that can include hands-on manual treatment, targeted coping strategies, and even the judicious use of passive modalities, physical therapists can have a great impact on acute and chronic pain, either helping patients to overcome the cause of that pain or giving them tools to minimize and cope with their pain.
4. Movement Education: Physical therapists have a unique roll as functional motor control experts. Whether the task is rolling over for the first time as an infant, regaining balance after a stroke, or finding the precise control to play football again after an ACL injury, physical therapists can rise to the challenge. Physical therapists understand how your body moves and can connect the dots between neural control, musculoskeletal strength, and the reality of each individual’s form to maximize human function.
5. Health Optimization: Rarely do paitents or clients of physical therapy make it through an encounter without gaining some benefit to their health apart from the condition or problem that got them there in the first place. It might be improved posture, it might be working out the tight hip that caused the low back pain in the first place, it might be the improved cardiovascular benefit of exercise, it might be a better understanding of how to manage their diabetes, or it might be reduced fear about re-injuring yourself. Physical therapists do much more than just fix body parts. They fix you!
Here’s what we need to remember. Physical Therapy is lucky enough to be a profession that does get mentioned on national press. Inherent in these two spots is something very strong and very important. It’s the idea that ‘Physical Therapists Fix You’. Even if the scholars of our profession squirm when the national media misses the mark on evidence-based treatments, the idea that physical therapists can take care of you is still very present, and very powerful. That is our true brand. And, I can live with that.
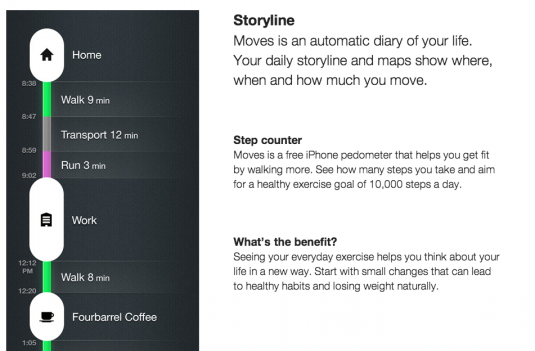 I wish I had this newly released app last week during CSM 2013! Moves by Protogeo Oy, brings a sweet new movement tracker to the field of personal data monitoring. With no need to purchase a new device, charge it, or risk losing it, Moves is a smartphone app that uses a combination of your phone’s accelerometer and some server-based processing to determine what you are doing and when. Cycling? Got it. Running? Got it. Driving to the next trailhead? Got it covered. This innovative solution highlights the capabilities of app development companies, showcasing how they can create tools that seamlessly integrate into our daily lives. (I wouldn’t swim…) with your phone…but…)
I wish I had this newly released app last week during CSM 2013! Moves by Protogeo Oy, brings a sweet new movement tracker to the field of personal data monitoring. With no need to purchase a new device, charge it, or risk losing it, Moves is a smartphone app that uses a combination of your phone’s accelerometer and some server-based processing to determine what you are doing and when. Cycling? Got it. Running? Got it. Driving to the next trailhead? Got it covered. This innovative solution highlights the capabilities of app development companies, showcasing how they can create tools that seamlessly integrate into our daily lives. (I wouldn’t swim…) with your phone…but…)





