No, you’re not entitled to your opinion. Well, so says lecturer in philosophy Patrick Stokes
I’m sure you’ve heard the expression ‘everyone is entitled to their opinion.’ Perhaps you’ve even said it yourself, maybe to head off an argument or bring one to a close. Well, as soon as you walk into this room, it’s no longer true. You are not entitled to your opinion. You are only entitled to what you can argue for.”
A bit harsh? Perhaps, but philosophy teachers owe it to our students to teach them how to construct and defend an argument – and to recognize when a belief has become indefensible.
Usually, agreeing to disagree ends a discussion. But, agreeing to disagree in order to facilitate true debate should actually initiate the discussion. Attack the message, not the messenger. It’s not personal.
And, that’s the point. Rigorously critiquing the message, ideas, and reasoning is not insulting the person. It’s the foundation of the evolution of the scientific process after new data or theories emerge. Heated, passionate debate can (and I would argue should) be followed by laughter and delicious beverages amongst colleagues (and even rivals!). These fiercely disagreeing colleagues can even be friends.
You are safe, but your ideas are not
But, we are dealing with humans. Humans with complex emotions, previous experience, and beliefs. Brains that are prone to cognitive biases and logical fallacies, even when explicitly on the lookout for them. We are a messy, social, complicated, emotional bunch. The online experience evolved to Web 2.0 “the collaborative internet” (now even Web 3.0) resulting in the proliferation of two way communication and information exchange on the web. The user is actively involved in collaboration and user generated content. Interaction with both content and people has become an integral, regular facet of the online experience. Blogs, blog comment sections, Facebook, and micro-blogging platforms such as Twitter are a routine part of our social as well as professional lives.
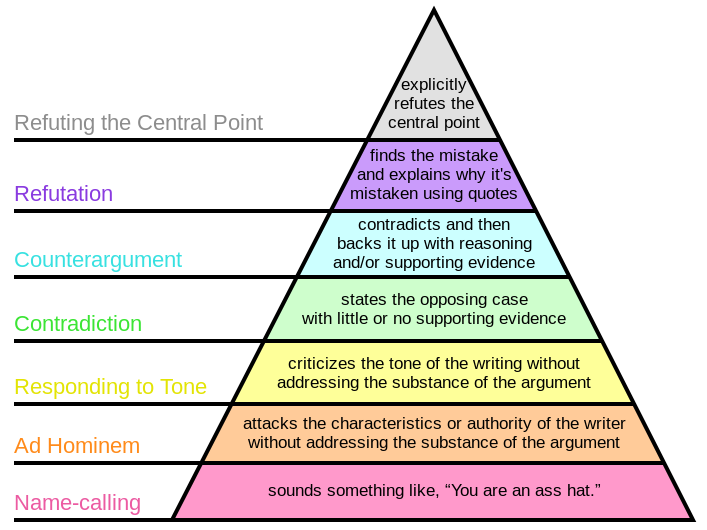
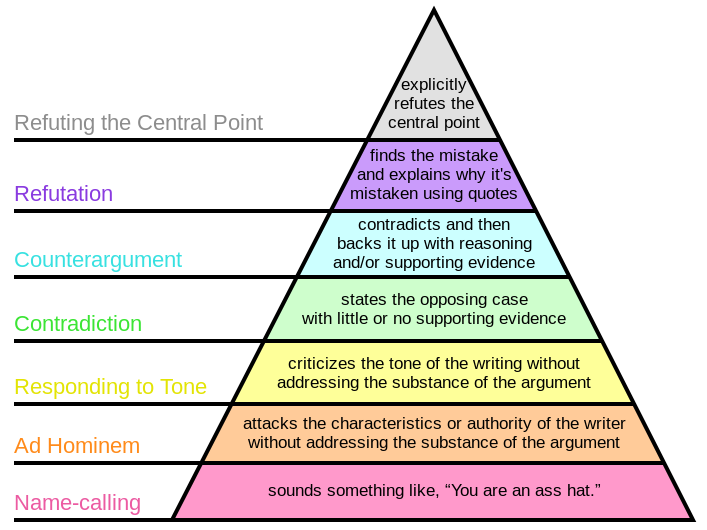
So, how can we foster real debate and discourse that is focused on the issues? It’s simple (kind of, in theory), but it’s not easy. Philosophically, absolute truth is a hard, if not impossible, concept (wikipedia truth). In discussions regarding both science and clinical care, the aim is not to be right (per se). But, rather, to approach a state of less wrong. Such a concept recognizes the evolving nature of our understanding in light of new evidence and insight. The goal thus becomes a proper analysis of the position or conclusion presented including the evidence (from basic science to outcomes studies) but also the logic, reasoning, and prior plausibility supporting or refuting the stated position. This approach applies to online discussion, article analyses, professional discussion, and education at all levels. The disagreement hierarchy outlines the strength, and relative validity, of a counterargument. It provides a formal guide for framing discussions.
Why is all of this important?
The online disinhibition effect describes how interactions online may actually be more prone to errors in disagreement and discussion. Whether on blogs, Facebook, or Twitter endless examples of poor debate are present. Ad homineum attacks (you have no experience in this), complaints of tone (you’re so negative), and down right insults (you’re an idiot). Gross illustrations of both logical fallacy and bias (we’ve all got it, except for me of course).
Sometimes, the lower levels of the disagreement hierarchy are actually true. An ad hominem argument highlighting an individuals lack of expertise, knowledge, or experience may be factually accurate. But, while true in and of itself, it does not necessarily invalidate or refute or counter argue the position presented. For example, a cranio-sacral therapist may argue that I have “no experience” performing cranio-sacral therapy. While true, that does not address my position that cranio-sacral therapy’s explanatory model is indefensible, regardless of the perceived or studied effectiveness of the treatment. Thus, even if it works, it does not work as theoretical presented. And, that is vitally important, and often missed construct, when discussing clinical care. Mary Derrick, @Mary_PT2013, previously addressed the use of clinical reasoning and critical thinking from a DPT student’s perspective.
Thinking, Fallacies, and Biases
Unfortunately, an understanding of the mechanics of debate and the basic fallacies of logic is not sufficient. In order to discuss effectively at a high level we also must possess critical thinking skills. We need to understand and recognize logical fallacies and cognitive biases. We need to understand the basic mechanics of science, mathematics, and statistics. We need to understand what certain studies can and can not tell us. We need to understand prior plausibility. We need to think about our thinking (metacognition).
Even more unfortunate is the lack of teaching students how to think. “Schools of thought” and “gurus” continue to dominate our profession as well as public discourse (see Dr. Oz and the muriad of health and fitness fads). Students, practitioners, and even researchers indoctrinated in evidence based practice volley outcomes based RCT’s attempting to illustrate their positions. Professionals argue with each other about tone, experience, and doing “whatever works.” As Jason Silvernail, DPT, DSc observed in his post EBP, Deep Models, and Scientific Reasoning
When I see my colleagues approaching alt-med treatments asking for outcome evidence, I get justifiably nervous – are they just one RCT away from believing in energy medicine? What we should be focusing on is the absolutely indefensible theory here – it’s scientific reasoning that will help us here, not statistics. Let’s never forget that.
Specifically as the profession of physical therapy and more generally in science and public discourse the conversations needs to continue beyond “lets agree to disagree.”
Debate and arguments need to occur
There are beliefs, models, terms, and ideas that permeate our profession, the health care system, and culture that need abandoning. Can you think of any? Understanding the what and why of clinical care and scientific discussion from a Science Based Medicine perspective:
Good science is the best and only way to determine which treatments and products are truly safe and effective. That idea is already formalized in a movement known as evidence-based medicine (EBM). EBM is a vital and positive influence on the practice of medicine, but it has limitations and problems in practice: it often overemphasizes the value of evidence from clinical trials alone, with some unintended consequences, such as taxpayer dollars spent on “more research” of questionable value. The idea of SBM is not to compete with EBM, but a call to enhance it with a broader view: to answer the question “what works?” we must give more importance to our cumulative scientific knowledge from all relevant disciplines.
If only it ended there. What about that uncomfortable feeling? Defensiveness, feeling offended, stomach churning. These feelings and thoughts are a result of your mind, your brain struggling with two conflicting ideas or ideals. Cognitive Dissonance
In psychology, cognitive dissonance is the discomfort experienced when simultaneously holding two or more conflicting cognitions: ideas, beliefs, values or emotional reactions. In a state of dissonance, people may sometimes feel “disequilibrium”: frustration, hunger, dread, guilt, anger, embarrassment, anxiety, etc.
Some studies illustrate that when presented with evidence conflicting their current position or understanding, humans actually become more entrenched in that belief or view point. So, without a focus and understanding on these principles of debate, disagreement, logic, and fallacy discussion poses the potential to be detrimental. The debate disintegrating into personal attacks and emotional based offensive points as each person drifts deeper into their current view point. Each party fighting uncomfortable cognitive dissonance, and actually confirming previously held beliefs. Critical thinking and metacognition are needed. Patrick Stokes again summarizes:
The problem with “I’m entitled to my opinion” is that, all too often, it’s used to shelter beliefs that should have been abandoned. It becomes shorthand for “I can say or think whatever I like” – and by extension, continuing to argue is somehow disrespectful. And this attitude feeds, I suggest, into the false equivalence between experts and non-experts that is an increasingly pernicious feature of our public discourse.
So, please, let’s agree to disagree.