Recently, @JasonSilvernail and I wrote a letter to the editor of the journal Manual Therapy entitled Innominate 3D Motion Modeling: Biomechanically Interesting, but Clinically Irrelevant. The article is currently in press [Reference: Ridgeway K, Silvernail J. Innominate 3D motion modeling: Biomechanically interesting, but clinically irrelevant. Manual Therapy (2012). doi: 10.1016/j.math.2012.02.017]. The letter was a response to a recently published article on the non-invasive 3-D modeling of SI joint and pelvic motion, which in our humble opinions lacked any clinical utility or relevance.
Our submission was denied prior to review 2 separate times because of word length. The (we feel arbitrary) word length for an editorial or letter to the editor is 500 words. Despite multiple e-mails explaining why our piece should be considered in it’s entirety, the editor (through the Journal manager) insisted on a 500 word maximum before being considered for review. The original submission was just over 1,100 words.
We were faced with some decisions. Increasing the scope of the piece to a different manuscript type such as a “masterclass” or “professional issue” was discussed. But, these pieces are usually 3 to 4,000 words and are beyond the scope of what we were trying to convey. We also debated about submitting to another journal, such as the Journal of Manual and Manipulative Therapy. In the end, we decided to cut the length to 500 words, publish our original piece (in it’s entirety) HERE on PT Think Tank, and start a discussion regarding the original topic as well as our current peer review and publishing system. We thought it was an ideal time to explore whether the current journal peer review system is working for clinicians and scientists and what, if anything, we should do about it.
The original piece can be found in it’s own blog post HERE. An excerpt is at the end of this post. Feel free to comment and distribute freely. We would love discussion surrounding the actual issues the letter raises, and some of our criticisms of the research.
In the end, our goal was to express our interpretation of the study Inter-tester Reliability of Non-invasive Technique for Innominate Motion by Adhia et al, including it’s relevance in the context of the current scientific research on the topic and modern clinical practice. We hoped to facilitate scientific discussion and discourse surrounding the topic. Yet, arbitrary word lengths and overly specific categorization of manuscript types actually hindered REAL discussion. For this, we are disappointed. We were not requesting 4,000 words in the journal for an unsolicited narrative review of an area not relevant to the readership. We were seeking consideration for an 1,100 word response letter to an article Manual Therapy had published. A response that in our minds was well written (you be the judge!!) and presented some key issues beyond the study itself that would be of interest to the readership.
We think it is likely that Manual Therapy and it’s editorial staff are forced into industry-standard practices that currently define the for-profit publishing industry. We have every confidence that the clinicians and scientists on the editorial staff of Manual Therapy are as interested in professional discourse as we are, but are hindered by the system. We do not doubt their scholarly curiosity or suggest any bias against us personally or our perspectives. In many ways they are as hindered by the system as we were. In fact, perhaps more so.
Many people feel the current medical publishing industry does not support clinicians and scientists, but in many ways is primarily about making money for publishing conglomerates. There are many well educated, well published scientists who have raised these concerns, including the people at Body In Mind. A group of scientists the New York Times featured is actually boycotting the publisher Elsevier. Interestingly, Elsevier publishes Manual Therapy. As again highlighted by the New York Times, the Office of Science and Technology Policy is currently debating the issue of access to publications, research, and data that are federally funded.
So, what are the problems?
Access. Most clinicians do not have access to the plethora of articles from countless journals across disciplines that could affect their practice. Thus, how are they supposed (or even expected) to provide evidence or science based treatment? Secondly, how are they to intelligently discuss the literature with other colleagues or scientists? At BEST, they are left to skim abstracts. Chad Cook, the editor of the Journal of Manual and Manipulative Therapy, discusses some of the biases and problems within the PT literature regardless of some these publication issues in his piece Don’t Always Believe what you read… on Joe Brence’s Blog Forward Thinking PT. How do you think research and readership biases are compounded when many (most?) clinicians have limited, if any access, to full text publications? Especially, when abstracts can drastically misrepresent not only the results, but clinical implications of a study. We highlight this issue in our letter regarding Adhia’s et al’s piece; the abstract and conclusions far outstep the data and study design.
Time. From submission to review to dissemination is a LONG process, especially for larger studies. Originally, we began work on our letter in the beginning of DECEMBER. Our first 2 submission were February 14th and 15th, with the final submission on February 24th. Our piece as accepted February 29th (yay leap year!!). Manual Therapy provided proofs for review March 14th. We are still unsure of when the letter will be electronically published. And, this is just for a 500 word letter to the editor!
Now, we fully understand the time required for adequate peer review in order to ensure proper scholarship and science in large scale trials that involve the presentation of large data sets and sophisticated statistical analyses. But, is there a better way? Does the current system allow for broad access, discussion, and connection? And, really, who benefits?
So, what needs to change?
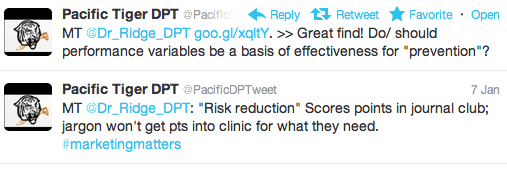
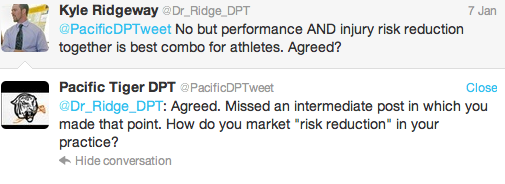
(Un)fortunately, more people will likely read, access, share, and comment on our original, longer piece published via this blog than the published letter to the editor in Manual Therapy. So, it appears the system is changing right before our eyes. The strength of Web2.0 is that discussion can happen right now. The process is dynamic as knowledge grows over time or people understand differently. I conceptualize this as real time peer review. Researchers, clinicians, students, and even those from other disciplines around the world can access and comment. This creates a vibrant, robust, and expert community of minds that are not limited by word count, publishing rules, or location.
A discussion on “Trigger Point Dry Needling” on @MikeReinoldBlog is an interesting case example. The post has generated 217 comments to date, some of them well researched, articulate, and publishable in our opinions! Imagine that type of discussion playing out in the literature of the current publishing system and paradigm? Unfortunately, the current literature at times is not as robust as these real time, remote, technologically driven interactions.
Fortunately, technology has afforded us the ability to highlight some of the pitfalls of the current publishing system, highlight our frustrations with our experience, and disseminate our original piece. Hopefully, this spawns discourse on scientific research and publishing, including open source and open access issues. Also, we would desire further discussion regarding the actual content of the research article as brought up in our response.
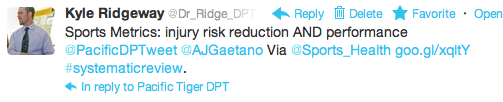
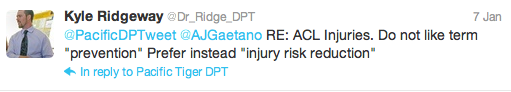
Interestingly, this entire project came about because of Web 2.0. Dr. Ridgeway stumbled across the abstract in his RSS feeder. It was e-published ahead of print. The article seemed out of step with the research evidence, and the author’s conclusions were in our opinion not supported by their study design and the current state of the literature regarding SIJ mechanics, treatment interventions, and lastly (but certainly not least) pain neurophysiology. So, @Dr_Ridge_DPT pushed a link of the abstract to both Twitter and Facebook. Dr. Jason Silvernail commented over social media and suggested a letter to the editor. The rest, as they say, is history. And oddly, despite their collegial nature Kyle and Jason have never met face to face! In total, 10 separate versions were created. The 10th version is the one that will be published in Manual Therapy at a mere 500 words. The 8th version, our best, can be read, in part, below:
We would like to thank Adhia and colleagues for their contribution to the literature regarding the non-invasive modeling of Sacro-Iliac joint (SIJ) motion. This study is interesting from a biomechanical perspective of the inter- and intra-rater reliability of measuring innominate motion via non-invasive palpation based measurements. However, in our opinion, this study has limited relevance to practicing clinicians and to the overall science and practice of manual therapy. The authors conclude “The results support clinical and research utility of this technique for non-invasive kinematic evaluation of SIJ motion for this population. Further research on the use of this palpation digitization technique in symptomatic population is warranted.” This seems to be a rather large logical leap given the results of their investigation and other data in the literature on the manual therapy assessment and treatment of the SIJ and pelvis region. We feel the clinical utility of SIJ palpatory movement testing has not been demonstrated by other research and we struggle to understand how such an assessment tool assists in evaluation, clinical assessment, or treatment with manual or physical therapy…CLICK HERE TO CONTINUE READING…
We thank you for reading, and urge you to comment with your views of the current publishing standard. In addition, what is your interpretation of the original Adhia et al article, and our reply?
@Dr_Ridge_DPT Kyle J. Ridgeway, DPT
@JasonSilvernail Jason Silvernail, DPT, DSc, FAAOMPT
Resources