Decades of clinical practice by manipulative providers have demonstrated the effectiveness of spinal manipulation as a therapeutic modality. The truth is that the mechanism of exactly how manipulation is effective has remained out of reach and unexplained. As research methods have become more sophisticated and the tool box of measures has increased in size, the prospect of figuring out a mechanism now seems a likely pursuit.
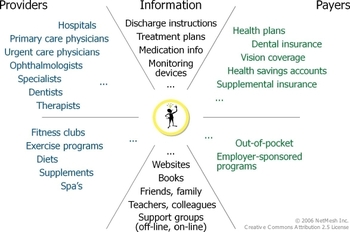
One handy tool that has become very popular in physical therapy research is ultrasonic imaging. Just like any ultrasound study, the clinician is able to observe real-time events. In the case of rehabilitative ultrasound imaging, the therapist is examining muscle activity. Measures of muscle thickness can vary and observable changes have been associated with pathology. For example, patients with low back pain show changes in cross sectional area of the lumbar multifidus muscle. Likewise, other patients with back pain have been shown to have difficulty activating their transversus abdominis muscle.
When this measure was used to study abdominal muscle thickness following a spinal manipulation procedure, an interesting thing occurred. The abdominal muscle activation changed! In a case series by Raney, Teyhen and Childs, spinal manipulation seemed to be correlated with a normalization of abdominal muscle recruitment patterns in patients with low back pain.
Perhaps this is a peek into the mechanism of spinal manipulation’s effects. The subluxation concept aside, spinal manipulation may have more to do with muscle activity, spinal reflexes, and the neuromuscular system than it ever had to do with alignment of the bones. The rapid, short duration of the motion used in manipulation does remind me of testing a deep tendon reflex!
Interesting to note, the researchers examined spinal manipulation in a group of symptomatic patients who met a criteria for a clinical prediction rule that identifies patients who are very likely to benefit from manipulation. Also interesting to note, this case series appeared after an initial case report by different investigators. They found a similar effect in another core stabilizer muscle in their report. Finally, we’re talking case report and case series here, so true causality regarding the phenomenon will have to wait for now.
This study is just one of many new investigations suggesting the role of spinal reflexes in the mechanism of manipulation. We will visit them over time here on the blog, along with some interesting off-shoots of that research.
Here’s the article abstract and citation:
Observed changes in lateral abdominal muscle thickness after spinal manipulation: a case series using rehabilitative ultrasound imaging.
STUDY DESIGN: Case series.
BACKGROUND: A clinical prediction rule (CPR) has been developed and validated that accurately identifies a subgroup of patients with low back pain (LBP) likely to benefit from spinal manipulation; however, the mechanism of spinal manipulation remains unclear. The purpose of this case series was to describe changes in lateral abdominal muscle thickness using rehabilitative ultrasound imaging (RUSI) immediately following spinal manipulation in a subgroup of patients positive on the rule.
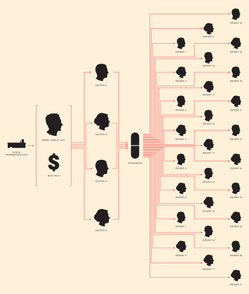
CASE DESCRIPTIONS: Data from 9 patients (5 female, 4 male; 18-53 years of age) with a primary complaint of LBP are presented. All patients had symptoms for less than 16 days (range, 3-14 days) and did not have symptoms distal to the knee, satisfying the 2-factor rule for predicting successful outcome from spinal manipulation. The Oswestry Disability Index scores ranged from 8% to 52%. Lateral abdominal muscle thickness was assessed with the patient at-rest and while contracted during an abdominal drawing-in maneuver (ADIM) using RUSI. Measurements were taken before and immediately after spinal manipulation. Patients completed a 15-minute training session of the ADIM prior to assessment, to mitigate the potential for a learning effect to occur.
OUTCOMES: Based on changes that exceeded the threshold for measurement error, 6 of 9 patients demonstrated an improved ability (11.5%-27.9%) to increase transversus abdominis (TrA) muscle thickness during the ADIM postmanipulation. Additionally, TrA muscle thickness at-rest postmanipulation decreased for 5 patients (11.5%-25.9%), while at-rest internal oblique muscle thickness decreased for 4 patients (6.4%-12.2%).
DISCUSSION: This case series describes short-term changes in lateral abdominal muscle thickness post spinal manipulation. Although case series have significant limitations, including the fact that no cause-and-effect claims can be made, the decrease in muscle thickness at rest and the greater increase in muscle thickness during the ADIM postmanipulation observed in some of the patients could suggest an improvement in muscular function. Future research is needed to determine if increased muscle thickness is associated with improvements in pain and disability and to further explore neurophysiologic mechanisms of spinal manipulation.
Citation:
Raney, N.H., Teyhen, D.S., Childs, J.D. (2007). Observed changes in lateral abdominal muscle thickness after spinal manipulation: a case series using rehabilitative ultrasound imaging.. Journal of Orthopaedic and Sports Physical Therapy, 37(8), 472-479.