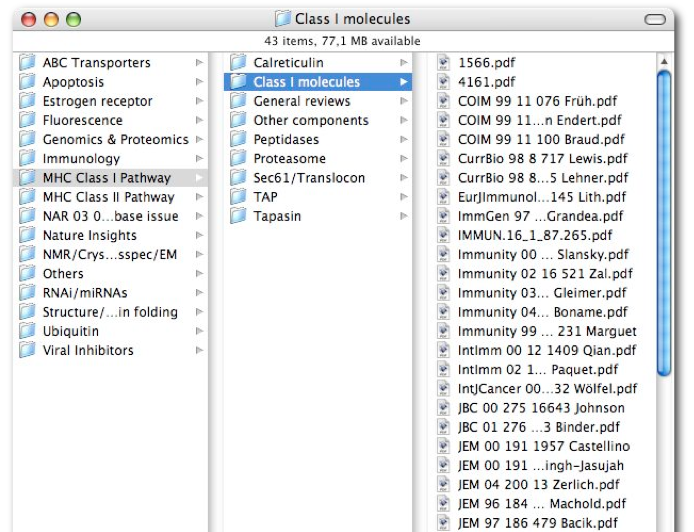
So, this series has had a long, long hiatus between posts for which I apologize!! Time to start the new year off right. This is another dense post with a ton of resources and links. I hope you enjoy. In the previous post, I presented which research journals publish the most and highest quality clinical trials of interventions. I also discussed what research journals we should consider following. The preceding posts in this series were:
- Web 2.0 and RSS
- Google Reader
- Selection of Content
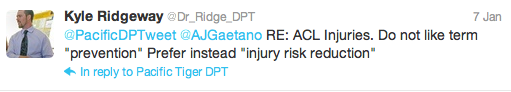
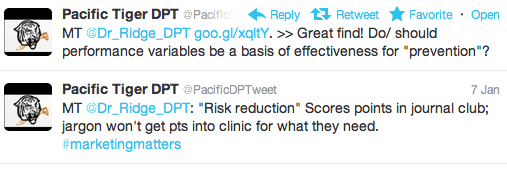
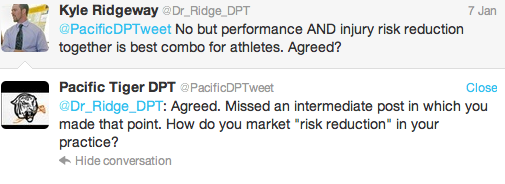
 But, research journals are not the only way for us to engage information relating to clinical practice and scientific research. Blogs are another great online resource. With the advent of Web2.0 principles physical therapists, students, and researchers from around the world can critique research, discuss science, and debate clinical practice through the blog format (And, the micro-blog format such as Twitter, but more on that in the next post!). Disagree with a bloggers interpretation of the evidence? Comment on the post! If utilized civilly and with proper logic blogs (and social media like Facebook and Twitter) are a great platform for learning, discussing, and reviewing. And, as I have mentioned in previous posts with RSS feeds the information is pushed directly to you. Then you decide what to skip, what to skim, what to read, what to push forward through Twitter or Facebook and what to comment on!
But, research journals are not the only way for us to engage information relating to clinical practice and scientific research. Blogs are another great online resource. With the advent of Web2.0 principles physical therapists, students, and researchers from around the world can critique research, discuss science, and debate clinical practice through the blog format (And, the micro-blog format such as Twitter, but more on that in the next post!). Disagree with a bloggers interpretation of the evidence? Comment on the post! If utilized civilly and with proper logic blogs (and social media like Facebook and Twitter) are a great platform for learning, discussing, and reviewing. And, as I have mentioned in previous posts with RSS feeds the information is pushed directly to you. Then you decide what to skip, what to skim, what to read, what to push forward through Twitter or Facebook and what to comment on!
There are many blogs relating to physical therapy, rehabilitation, training, science, exercise science, training, and research. I stumble upon new ones all the time. Some of them are great, some are bad, and some are just ugly. Below I am going to review some of the blogs that I follow.
I love the interactive nature of the blog format. You can participate in high level discussions regarding research and clinical practice from anywhere in the world. This type of crowd sourcing has the potential to elevate our knowledge dissemination, discussion, and growth. In fact, the proliferation of blogging and micro-blogging will (I believe) fundamentally change not only how information is disseminated, but how we learn, discuss, and collaborate on clinical care and research.
For each blog, I have included the title/subtitle hyperlinked to the actual blog as well as the author(s) twitter handle with a hyperlink to their twitter profile. Please comment on your thoughts of these blogs.
What blogs do you follow? Let us know in the comments section! Speaking of, follow @PTThinkTank as well as all the authors, including the creator @EricRobertson and humble contributors @MPascoe and @Dr_Ridge_DPT
I have to start off with some student blogs. As a student this is how I became exposed to and involved with leveraging technology!
AAOMPT sSIG: Blog of the Student Special Interest Group of AAOMPT
The AAOMPT sSIG Blog is where I got my start blogging about such issues as the doctor of physical therapy degree, direct access, physician owned physical therapy services, and grass roots political advocacy. The blog provides information on the happenings of the student special interest group. If you are a student, or know a student, send them to the blog for more information on getting involved in the sSIG. It is a great group of motivated, high energy students. Unfortunately, the AAOMPT sSIG is not on twitter, but you can e-mail the students directly with comments, suggestions, and questions: ssigaaompt@gmail.com
Colorado Student Physical Therapy Advocacy: Act now to protect the future of your profession
Author: @COSPTAdvocacy
I may biased since these students are from my Alma Matter, but these students are truly organized and accomplished. Not only did they WIN the APTA’s Student Advocacy Challenge they are leveraging technology through Blogger, Twitter, and Facebook to create a sustainable and visible student movement.
Below are some of the blogs that I regularly read and definitely have in my RSS Feed. Most of them deal directly with physical therapist practice, and are authored by physical therapists. Others are authored by other professionals, but still very applicable to physical therapy. Enjoy!
Better Movement: Learn to Move with More Skill and Less Pain
Author: @ToddHargrove
Todd is a Seattle based Feldenkrais Method movement instructor who used to be a lawyer. He writes about a neurocentric approach to movement, training, and pain. In Both Sides Now, he discusses research investigating the training, or treating, one side of the body and the effect on the contralateral side.
Body In Mind: Research into the role of the brain in chronic pain
Authors: @bodyinmind @NeilOConnell
This is the blog of Lorimer Mosely and crew out of Australia. They provide research summaries and discussions regarding the mechanisms of pain and the treatment of chronic. Probably one of the most robost blogs on the net regarding pain physiology and current research. Why Things Hurt is an outstanding Tedx video by Lorimer Moseley on the neurophysiology of pain. They even discuss if Chronic Pain is a Disease.
Categories: Pain Science, Chronic Pain, Neuroscience, Physiology, Research
Leaps and Bounds: Perspectives from a physical therapist
Author: @ForwardMotionPT
Corey provides unique insight into physical therapist practice, and is obviously a very deep thinker. He has produced many videos illustrating the use of novel movements of various body regions. Here is a great post about The Movement Diet.
HealthSkills: Skills for health living for health professionals working in chronic pain management
Author: @adiemusfree
Healthskills is a blog for health providers who want to read about research related to self managing chronic pain. Topics include chronic behavior therapy, measuring outcomes, patient education, and many other topics. The author was originally trained as an occupational therapist. In this post, she discusses what to do when a patient is “inconsistent” with their pain behavior or presentation.
Categories: Pain, Chronic Pain, Cognitive Behavior, Clinical Treatment of Pain
The Manual Therapist: Promoting the highest level of physical therapy practice
Author: @The_OMPT
Dr. E posts very regular providing links to other blogs (including this one, thank you!), videos on techniques he uses, clinical cases, and clinical reasoning. He has a very expansive background being both a fellow of AAOMPT and MDT diplomat. See the post What is the Mechanism Behind Rapid Change? for a discussion we had regarding mechanisms of manual therapy. (Here is the comments section)
Mike Reinold: Rehab | Sports Medicine | Performance
Author: @mikereinoldblog
The most up to date information related to evaluation and treatment of athletes, specifically overhead athletes. Good citation of clinical research for evaluation and exercise treatment. Lots of links to different courses/products. Mike is the head of athletic training for the Boston Red Sox, and is well published on issues regarding the shoulder and injuries in throwers. In the post Rotator Cuff Fatigue Increases Superior Humeral Head Migration, Mike discusses the importance of not training the cuff to fatigue.
Categories: Athletes, Shoulder, Knee, Sports, Orthopaedics
Move It: The New Professional’s Collaboration Blog
A group of young physical therapists (<5 years experience) discuss clinical practice, clinical development, and issues regarding being a new professional. It has been a while between posts, but they have some excellent content. Check out A Generation with Challenges, Vision, and Debt.
Categories: Young Professionals, Professional Development, Legislative Advocacy, Professional Issues
My Physical Therapy Space: Evidence in Motion Blog
Authors: @EIMTeam
The blog of the Evidence of Motion crew. Great information regarding private practice, legislative issues, and research pertaining to orthopaedics. Discussions regarding the overuse of imaging and surgery, as well as the how physical therapists can provide value to society and healthcare. In a Blast from the Past, John Childs illustrates how some clinicians and researchers cling to old models of pain and treatment despite evidence to the contrary. Tim Flynn discusses how access to early, cheap care (physical therapists!) for low back pain is Not Rocket Science, and could have HUGE implications for our society. Larry Benz deconstructs poor logic about Physician Owned Physical Therapy Services (POPTS) that appeared in Advance Magazine.
Categories: Professional Issues, Private Practice, Orthopaedics, Research, Professional Development
The Sports Physiotherapist: Resource for physiotherapists (or physical therapists) with a passion for assessing, diagnosing, and rehabilitating the sports injuries of the world’s athletes
Author: @TheSportsPT
Extremely well cited articles discussing the evaluation, assessment, and treatment of athletes including surgical approaches and their implications on rehabilitation. Their blog and website is maybe the most comprehensive sports physical therapy resource on the net. In this post, they review the diagnostic accuracy of tests used to identify Acetabular Labral Tears of the Hip.
Categories: Sports, Athletes, Research, Examination
Physical Therapy Diagnosis: Make Decisions Like Doctors
Author: @timrichpt
Private practice owner in Florida discusses clinical decision making as well as leveraging decision support tools/software. Lots of discussion of Medicare flaws, clinical decision making, and issues in private practice. Tim recently authored a book detailing bullet proof decision making processes to improve documentation and efficiency in outpatient practices. Tim presents The Art and Science of Physical Therapy by analyzing the Oxford Debate from the American Physical Therapy Association’s Annual Conference in 2011
Categories: Private Practice, Legislative Issues, Clinical Decision Making, Outpatient
Save Yourself: Science powered advice about your stubborn aches, pains, and injuries
Author: @painfultweets
A massage therapist by training who turned to science focused blogging regarding painful problems. Skeptical analysis of pain, pain syndromes, and treatment techniques. Great information for patients and practitioners alike. Although I very much respect Paul’s work and critiques, there is a very apparent bias towards trigger points as a significant pain complaint and treatment target. Paul talks about MRI Overuse and how MRI is too sensitive of a diagnostic tool. He also does a nice job of summarizing some of the Science Surrounding Stretching.
Categories: Pain, Chronic Pain, Manual Therapy, Science
SomaSimple: The so simple body. A place for physical & manual therapy.
@SomaSimple Contributors: @jasonsilvernail @dfjpt @BarrettDorko @wrtrohio @JohnWarePT @ForwardMotionPT among others
You will not find a more thorough or logical analysis of manual therapy, physical therapy, and their relation to people with painful problems anywhere. The folks over there are true skeptics in their thought process, and challenge all. Be ready to be challenged, even if all you do is read the forums! This site is such a density of information and discussion you could read for months. Whether you troll or join in on the discussion it will deepen your analysis and understanding of pain, pain physiology, and clinical practice. Enough is Enough is a well written piece by Jason Silvernail talking about how we need to stop looking for the magical technique or tissue and focus on deeper models of understanding pain. In Crossing the Chasm, he absolutely shines in his ability to tie current clinical research to a deeper, neurophysiologic understanding of pain as he describes his process of evaluation and treatment utilizing sub-grouping in low back pain.
Categories: Pain, Neuroscience, Discussion Board, Manual Therapy
The blogs above are more specific to physical therapy principles. But, it also useful to engage information from other disciplines or sources. For example, decision making, principles of science, behavior, and psychology are all integral parts of physical therapy practice. These topics relate to how we treat patients, but maybe more importantly how we make decisions and analyze/integrate literature.
Science Based Medicine: Exploring issues and controversies in the relationship between science and medicine
I believe this is a must read blog for all health care professionals. It discusses the application of scientific principles to improve evidence based practice. These principles include prior plausibility, physiologic plausibility, and an increased focus on the integration of basic science into the understanding and practice of medicine. Although, much of it is not related directly to physical therapy, the lessons and principles discussed are applicable to research interpretation and clinical practice of all health care professions. In fact, physical therapists receive a mention in the post Subluxation Theory: A Belief System that Continues to Define the Practice of Chiropractic.
Check out these posts:
- About Science Based Medicine
- Announcing Science Based Medicine Blog
- Does Evidence Based Medicine Undervalue Basic Science and Overvalue Randomized Control Trials?
- Is it a Good Idea to test Highly Implausible Health Claims?
Eric Cressey: Performance and health on a whole new level
A personal trainer with a masters degrees in kinesiology with a highly successful persontal training facility targeted towards baseball players. Collaborates with Mike Reinold. Although targeted for personal trainers and fitness specialists, he provides amazing information on training athletes that is very applicable to physical therapists.
Very detailed information about the training of high level athletes especially baseball players. Eric exhibits in depth understanding of kinesiology, training, and anatomy specifically as it relates to baseball players and overhead athletes. Although, he does seem to have a poor understanding to mechanisms and effects of manual therapy and at times “plays doctor” in regards to client’s pain complaints. In How Much Rotator Cuff Work is Too Much? Eric discusses the implications of training the rotator cuff in throwing athletes both in season and during the off season. He highlights the fact that many throwers overuse their cuff musculature.
Categories: Sports Training, Baseball, Shoulder
- Do you read any of the blogs above? If so, what is your critique?
- Did we miss a good resource? Please comment and enlighten us!
- Do you have a blog? Comment with a link and a brief summary!
Unfortunately, there seems to be a lack of physical therapist focused blogs relating to in-patient acute care, neurologic physical therapy, and in-patient rehabilitation (hint, hint, any takers??). Most focus on outpatient, orthopaedics, sports, and private practice.
I hope you have enjoyed the leveraging technology series thus far! We have covered a ton of information as these posts are are very dense. The next post will discuss the use of social media tools including Twitter, Facebook, and Blog comments to move beyond RSS into active sharing, discussion, and engagement of information! Remember, we always value your feedback and comments.
@Dr_Ridge_DPT