All you do is walk people! Are you going to walk Mrs. Smith? Are you getting Mr. Johnson up? You don’t have to think in acute care!
In my opinion, the role of the physical therapist in acute care hospitals has some of the most profound & robust reasoning and logic. In addition, clinical research evidence continues to illustrate the positive benefit of physical therapists within acute hospitals for individuals who have had total joint replacements to the most critically ill individuals in intensive care units. The Physical Therapy Journal special issue on Rehabilitation for People with Critical Illness inspired me to discuss acute care practice in more depth. Despite the complex, fast paced environment and short lengths of stay, physical therapists continue demonstrate value in regards to patient outcomes, hospital throughput and flow, and risk reduction. The acute care environment is bursting with opportunity for physical therapists to enact meaningful change through innovative practice models and health care changing research.
Yet, the above are common statements and questions the acute care physical therapist must routinely face. Unfortunately, the skills, knowledge, role, and contribution of the acute physical therapist is misunderstood not just by other healthcare professionals within and outside the hospital environment. Equally as important, is the misunderstanding of physical therapist colleagues who practice in other settings.
In the editorial Acute Care Physical Therapist Practice: It’s Come a Long Way physical therapy journal editor Dr. Rebecca Craik, PT, PhD, FAPTA comments:
“Should Physical Therapists Practice in Acute Care Settings?” That was the 2007 topic for the Rothstein Debate, an annual event held at APTA’s conference and exhibition and established to honor PTJ’s esteemed Emeritus Editor in Chief Jules M. Rothstein (1945–2005).
Dianne Jewell, PT, PhD, FAPTA, was moderator. Anthony Delitto, PT, PhD, FAPTA, and Charles Magistro, PT, FAPTA, argued for and against the need for physical therapists in the acute care setting. On one side, the physical therapist was characterized as a sophisticated decision maker with a breadth of knowledge that spanned medicine and physiology; on the other side, the physical therapist was characterized as just another clinical staffer who “dragged” patients down the hall.
The session was filled to capacity with approximately 300 people; the tension was palpable, the debaters articulate—but tempers were kept in check. The debate was declared a draw. I still recall my surprise that day at learning about the paucity of research on acute care practice:
1. The clinical decision-making process touted as complex by the “pro” team had not been described in the literature.
2. Responsive outcome measures had not been agreed upon.
3. Clinical trials had not been conducted to compare different interventions in that setting.
4. Cost-effectiveness had not been examined.
Today, in my opinion, I feel asking whether physical therapists belong in acute care shows a gross misunderstanding for the history and future of the physical therapy profession generally and the role of the acute care practioner specifically. Where is the recognition and assessment of the logic, rationale, and research behind acute care practice? My hope is that this debate topic was purposefully chosen to expose physical therapists to the acute care practice environment. Dr. Craik contends it inspired action. Acute care research and investigations since that debate have grown tremendously in both number and quality.
What are the physical therapist’s roles in acute care?
The obvious role of the physical therapist is to examine and evaluate a patient within the International Classification of Functioning, Disability, and Health (ICF Framework) to determine current and future need for rehabilitation, appropriate discharge location, equipment needs, and current functional level. Specific impairments of body structures and function, activity limitations, and participation limitations can be identified. Physical therapists can then also prescribe mobility and movement recommendations which I like to term “movement medicine.” This conceptualization of acute care practice, while accurate, is overly simplistic. For many, this is where their understanding and conceptualization of #acutePT ends. In fact, it only represents a minute fraction of the effect and role of PT.
Beyond Function…
The profound effect that physical therapists can have in the acute care environment extends far beyond function and mobility. When analyzing the acute care practice environment from the outside many often ask if specific physical therapy interventions are effective from a functional, patient outcomes standpoint. While valid, this narrow scope does not fully encompass acute care practice.
The role and effect of the physical therapist’s presence, input, and treatment (generally and intervention content specifically) needs to be analyzed from multiple perspectives. Various metrics need to be assessed. Outcomes from multiple levels of the care and delivery process from the individual patient to the specific unit to the hospital to the entirety of the healthcare system need to be analyzed. This includes not only function and functional improvement, but current and future costs of an episode of care. No doubt, patient performance and function including future functional status and time to accomplishment of functional milestones are vitally important. But, length of stay, readmission rate, proper/safe discharge location, and reduction of medical complications are all important outcomes to patients, hospitals, and the healthcare system.
Physical therapist’s presence, guidance, and treatment can actually reduce the risk of adverse medical events including pneumonia, blood clots, readmissions, and longer lengths of stay. They may have an impact on hospital costs, future medical costs, overall healthcare costs and morbidity. These are important outcomes metrics. Taking a function only approach to acute care physical therapist practice and research may be detrimental. For example, a study may show that the functional outcome of a patient population treated by a physical therapist resulted in minimal improvements in function at hospital discharge. But, what if the same study illustrated that the treatment drastically lowered the incidence of pneumonia. Is that an outcome of interest to patients, physicians, hospitals, and health care administrators? A retrospective study illustrated physical therapists make accurate and appropriate discharge recommendations. More interestingly, when actual discharge location did not match the therapist recommendation the odds of readmission were 2.9 times higher than when the actual discharge matched therapist recommendation.
Physical therapists act not only as treating clinicians, but valued consultants (or a consulting service) in the acute care hospital. In a qualitative study of acute care practice the authors discuss acute care physical therapist practice in the evolving healthcare and hospital environment
According to the Centers for Disease Control and Prevention’s National Center for Health Statistics, the number of hospital days of care for patients of all ages was 226 million in 1970 compared with only 166 million in 2006. Similarly, the average length of stay was 7.8 days in 1970 and 4.8 days in 2006. Today’s hospital environment is one where patients are admitted for procedures, invasive medical management, and surgical interventions while longer-term healing, recovery, and rehabilitation occur elsewhere.
As a result, questions have been raised regarding the relevance of physical therapist intervention and management, commonly associated with the more lengthy rehabilitation phase of care, being delivered in such a fast-paced setting. The responses of the physical therapists interviewed in the study by Masley and colleagues suggest something else is occurring. The themes of this article and previous studies regarding the role of the physical therapist seem to demonstrate that physical therapists have evolved to becoming valued professional consultants who provide a unique, essential perspective, rendering them integral contributors to the acute care team. Today’s physical therapists specialize in evaluating and managing the patient’s functional mobility needs and, within that scope, serve as both consultants and effective transitional care providers.
Communication and Advocacy
Inter-professional communication is an ongoing necessity within the acute care hospital. Physical therapists are routinely interfacing with nurses, physicians, case managers, social workers, and other hospital staff. Acute care physical therapists are positioned to find and fight for allies outside the physical therapy profession. Emergency medicine and critical care physicians are recognizing the skills, expertise, and contribution of physical therapists. From coast to coast, they are advocating for physical therapists within and outside hospital walls resulting in development of innovative clinical programs and lines of research. Physical therapists are routinely a part of trans-disciplinary programs to improve patient care and outcomes. Through their physical location within a hospital setting, acute care physical therapists can leverage knowledge, skills, and expertise to promote and advocate for the entire profession of physical therapy.
Where’s the evidence?!?!
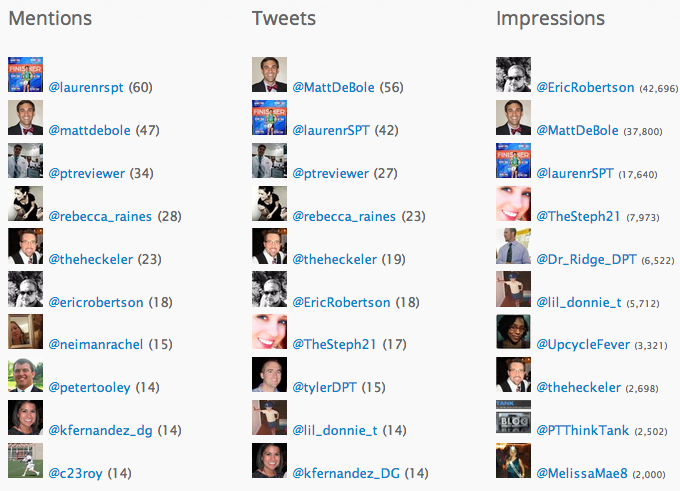
Recently, on twitter, a #DPTstudent tweeted that acute care had the least amount of supporting research. One of the reasons for this perception, I believe, is that much of the evidence supporting physical therapist practice in acute care is published in non-physical therapy specific journals such as Critical Care Medicine, Chest, and the Archives of Physical Medicine & Rehab. For example, Critical Care Medicine published an entire supplemental issue on Intensive Care Unit-Acquired Weakness (ICU-AW). But, the Journal of Acute Care Physical Therapy and Cardiopulmonary Physical Therapy Journal are still fantastic resources (by jennifer). As I outline in the Leveraging Technology Series post Selection of Content, we must read outside of the physical therapy specific literature. So far, I have discussed some of the rationale, which is vital, but what has research illustrated?
Total Joint Replacement
A study investigated the effect of immediate postoperative physical therapy on length of stay for total joint arthroplasty patients illustrating that “Isolated PT intervention on POD 0 shortened hospital LOS, regardless of the intervention performed.” A study published way back in 1993 illustrated that receiving weekend treatment by a physical therapist correlated with decreased length of stay following joint arthroplasty.
Emergency Department
I have written before about the emergence of physical therapists in the emergency department. Preliminary data illustrates potentially improved patient satisfaction with care and shorter wait times when physical therapists are present in the ED. In addition, physicians practicing in emergency medicine have recognized the expertise and contribution of physical therapists in a variety of conditions including painful problems, musculoskeletal conditions, dizziness, and overall mobility/safety/discharge determination. An article in PTJ discussed the development of this novice practice venue.
Intensive Care Units
“Intensive Care Units cater to patients with the most serious injuries and illnesses, most of which are life-threatening and need constant, close monitoring and support from specialist equipment and medication in order to maintain normal bodily functions.”
Early mobility and physical therapy has been shown to be not only safe, but feasible in the individuals who require mechanical ventilation. A randomized control trial investigating early physical therapy and occupational therapy in critically ill mechanically ventilated patients concluded that not only was early physical therapy treatment safe and well tolerated early on in a critical illness course, but resulted in better short term functional outcomes and less delirium. Early physical medicine and rehabilitation for patients with acute respiratory failure: a quality improvement project demonstrated with “hospital administrative data…that across all MICU patients, there was a decrease in intensive care unit and hospital length of stay by 2.1 (95% confidence interval: 0.4-3.8) and 3.1 (0.3-5.9) days, respectively, and a 20% increase in MICU admissions compared with the same period in the prior year” And earlier this year, a systematic review on early mobility in the intensive care unit was published.
Response Dependent Progression
Back to some of the original questions. Well, so what? All you are doing is helping people get up and walk around. Can’t a nurse assistant do that? In a study of mobilization level in a surgical intensive care unit it was found that physical therapists mobilize their patients to a higher level than nurses. And, sometimes sitting ain’t easy. What appears simple procedurally often involves complex knowledge and decision making. A gentle manual technique may require a complex reasoning process and constant assessment of patient response. Similarly, in acute care the decision to sit up, stand, transfer, or ambulate requires the integration of physical therapy specific principles with knowledge of medical conditions, medical management, pharmacology, and pathophysiology. Mobility and therapy progression (within and between session) is based upon the principle of response dependent progression which necessitates integrating the previous knowledge with the patient’s current presentation/functional status while constantly monitoring physiologic status (vital signs), patient performance, and patient feedback (fatigue, shortness of breath, and other symptoms). The acute care physical therapist must assess and integrate complex information from various sources. Much of this information is dynamic in nature requiring constant integration and re-assessment…
So, you think you can walk?