Earlier this year I had a very positive experience attending my first physical therapy conference – CSM 2011, in New Orleans, LA.
Twitter was instrumental in the success of my experience. I thought I would take a moment to show you what I did leading up to the conference. Using twitter, I was able to break-the-ice with several attendees in advance so that when I got to the event I had several conversations waiting to happen.
Use this post as a checklist to prepare for your next PT conference. For me this will be the 2011 AAOMPT Annual Conference, Oct 26-31 in Anaheim, CA.
1. Create your twitter account
- Choose your name carefully. You want to avoiding changing your name down the road as this will force your followers to find you again once the change is made
- Choose a name that represents the content of your tweets – JSmithDPT for professional content; JoeSmith22 for personal; XFactorPT for clinic content, etc…
- Really consider including PT or DPT in your twitter name, especially if you’ll be tweeting about #physicaltherapy
- Enhance your profile. Add a picture, write a brief biosketch (you are limited to 160 characters), add your location, paste in your homepage URL (university profile, facebook page, a zapd page, etc…)
2. Follow other people on twitter by mining a twitter list
- Twitter has a way you can group twitter profiles with a common interest called lists
- If you find someone has created a list of conference attendees, you can view the list and find some interesting people you can start following and maybe even reach out to
- Here’s the list I’m putting together for 2011 AAOMPT Annual Conference
- This is a good way to find people on twitter because someone else has already done all the work for you
- You might also want to check out my list of physical therapy related twitter accounts and ask me to add you if I haven’t already
3. Create your own twitter list
- Once you have seen the usefulness of a twitter list, I suggest you start your own for the conference
- Start looking for people you know or would like to get to know by using the “Who to follow” feature
- Also search for an official conference account and add that to your list – AAOMPT actually has one
- If you find the conference organizer has an account, your can also mine their followers, here are the >1,000 people that follow @AAOMPT, do any of them look familiar to you?
4. Search twitter
- Twitter is a powerful way to find information instantaneously about topics you’re interested in, so start searching for content related to your conference, “AAOMPT” for example
- For large conferences, attendees will include a hash-tag to specify that their tweet is related to the conference, such as #AAOMPT11 or #CSM2012
- As you find people tweeting about the conference, add them to your list
5. Broadcast your plans
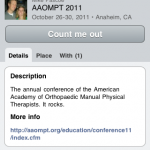
- Let your colleagues know you are planning on attending a conference by using the service called plancast
- Plancast connects to your twitter account and allows you to see what others are planning to attend
- Here is my account on plancast, showing that I am planning on attending AAOMPT11
6. Even if you’re not going
- Watch the hash-tag (#AAOMPT11) to see what people are sharing
- Ask questions, say hello
- Help promote the event by tweeting: “hearing lots of good chatter from #AAOMPT11 this week!”
7. Go mobile!
- Everything mentioned above can be done in a browser on a laptop or desktop computer, however, I found that I was much more likely to interact with twitter from my smart phone
- In fact, I barely looked at twitter for the first 6 months I had my account. It wasn’t until after I got setup on my iPhone 3GS that I really got immersed
- The screenshots in the gallery below were all taken from the iPhone app Tweetbot ($2.99 in the app store), but I suggest trying the free Twitter for iPhone app first (those on other smart phone platforms can chime in with links to your favorite apps in the comments below)
- Plancast also has a free mobile app
- It is also easier to share photos from your smart phone, assuming most smart phones have a camera these days
- One free photo sharing app that is on fire right now is instagram, which also connects to your twitter account
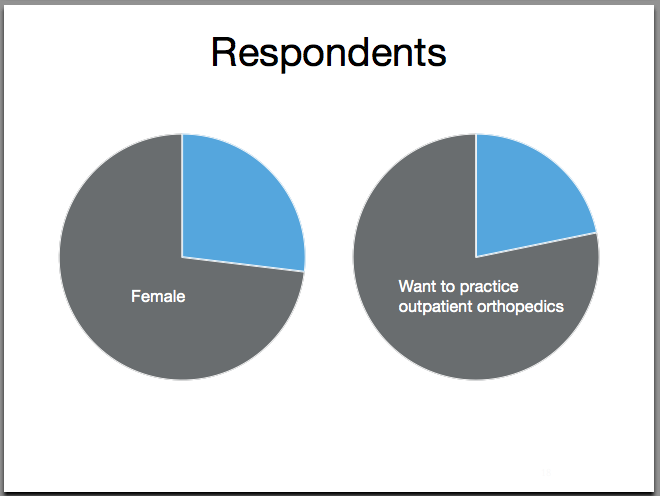
Gallery of screen shots from my iPhone shows some of the features mentioned above:
In closing…
I hope this was helpful and easy to digest. As usual, we want your feedback on this post in the comments – what did you like, what was explained poorly, what is your story with twitter at PT conferences, did I leave anything out, etc…
If you’d like to read more about social networking in physical therapy, I suggest reading this recent article on the Australian Physiotherapy Association website – “Why social media matters for physiotherapists”
Mike Pascoe – @mpascoe