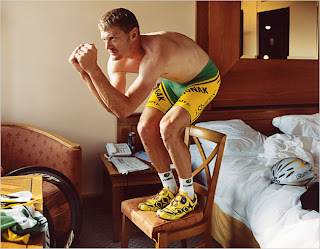
 Ok, first a disclaimer: I like cycling. I coach cycling. I like when Americans win cycling events. I liked everything I knew about Landis except that he left the Discovery Team to race for Phonak. I think there is no sport more corrupt, backwards, and overall annoying than cycling. I do not trust Anti-doping agencies, in that they only get budgeted by convicting people. In other words, my personal bias is to not believe most of the recent press about doping in cycling. Finally, and obviously, I am not an endocrinologist or doping expert.
Ok, first a disclaimer: I like cycling. I coach cycling. I like when Americans win cycling events. I liked everything I knew about Landis except that he left the Discovery Team to race for Phonak. I think there is no sport more corrupt, backwards, and overall annoying than cycling. I do not trust Anti-doping agencies, in that they only get budgeted by convicting people. In other words, my personal bias is to not believe most of the recent press about doping in cycling. Finally, and obviously, I am not an endocrinologist or doping expert.
Good. Now, let’s have a discussion. As background for our discussion, I will direct you to an excellent blog post on the science behind Floyd’s positive test at Jake Young’s Pure Pedantry blog. It’s a great overview of the case. Next, I also recommend the blog, Trust but Verify, which is dedicated to covering the events of this case.
An excerpt from Pure Pedantry:
"There is a very legitimate question related to the timing of the positive test. Floyd Landis tested positive on day 17 of the Tour de France — right before he made a miraculous comeback to retake the lead. Some people may speculate that testosterone may have helped him do this. This is unlikely to be the case. Testosterone is used during training periods to gain muscle mass. It is not a stimulant like amphetamines. It is not likely that testosterone would improve performance on such a short time scale, nor has it ever been shown to have that effect."
And that is the most poignant question: Why would all the tests he took during the Tour be negative except for one?
Yesterday during his hearing, defense expert Dr. John Amory had the same concerns:
"The case didn’t make a lot of sense to me," Amory said. "Initially when I saw the documents, I thought there were irregularities, first with the handling of the samples, then with the results."The ratios went from 1.5-to-1 and 1.8-to-1 to 11-to-1, then quickly back below 2-to-1 over the span of 10 days.
"I don’t consider those results to be consistent with the use of testosterone gel over that period of time," Amory said.
The only thing I have read that could even come close to offering an answer to this is that testosterone could potentially hasten recovery. This is exactly what the USADA (U.S. Anti-Doping Admin.) tried to argue with the
testimony of Joe Papp, a former low-tier pro and convicted doper. His testimony got a lot of press and I cannot understand why. This case represents the career and reputation of a man on the line. Yet, the prosecution sees fit to attempt to make a case on the subjective reports of one guilty cyclist about the effects of a testosterone gel on his recovery.
So What Do I Think About Landis?
It doesn’t matter what I think. The facts of the case are what matters. I do think one must question the strength of any case which is going to rely on non-blinded testers and subjective single case reports!
That’s not really science, now is it?Labels: current press, Questionable Practices, sports
 Here is an article about Oscar Pistorius of South Africa, who is petitioning to be allowed to run in the Olympics with two below-the-knee prosthesis. He is, by far, the best para-olympic runner. His time in the 400 is good enough to win the women’s event at the last Olympics. However, rules are rules and there is now a debate about whether or not he should be allowed to run.
Here is an article about Oscar Pistorius of South Africa, who is petitioning to be allowed to run in the Olympics with two below-the-knee prosthesis. He is, by far, the best para-olympic runner. His time in the 400 is good enough to win the women’s event at the last Olympics. However, rules are rules and there is now a debate about whether or not he should be allowed to run.