PT Think Tank is proud to announce that over the coming weeks leading up to the NEXT Conference and the annual House of Delegates meeting, we will be covering all proposed motions in detail. These motions by nature are complex and have taken enormous amounts of effort and time from the authors and the Reference Committee to compile. Our goal is to provide insight and high-quality background information to these motions and begin a conversation about how these motions if accepted, could change our everyday practice of Physical Therapy. In order to effectively understand the motions that are being presented for the 2017 HOD, we must first understand how motions are developed, organized, and presented.
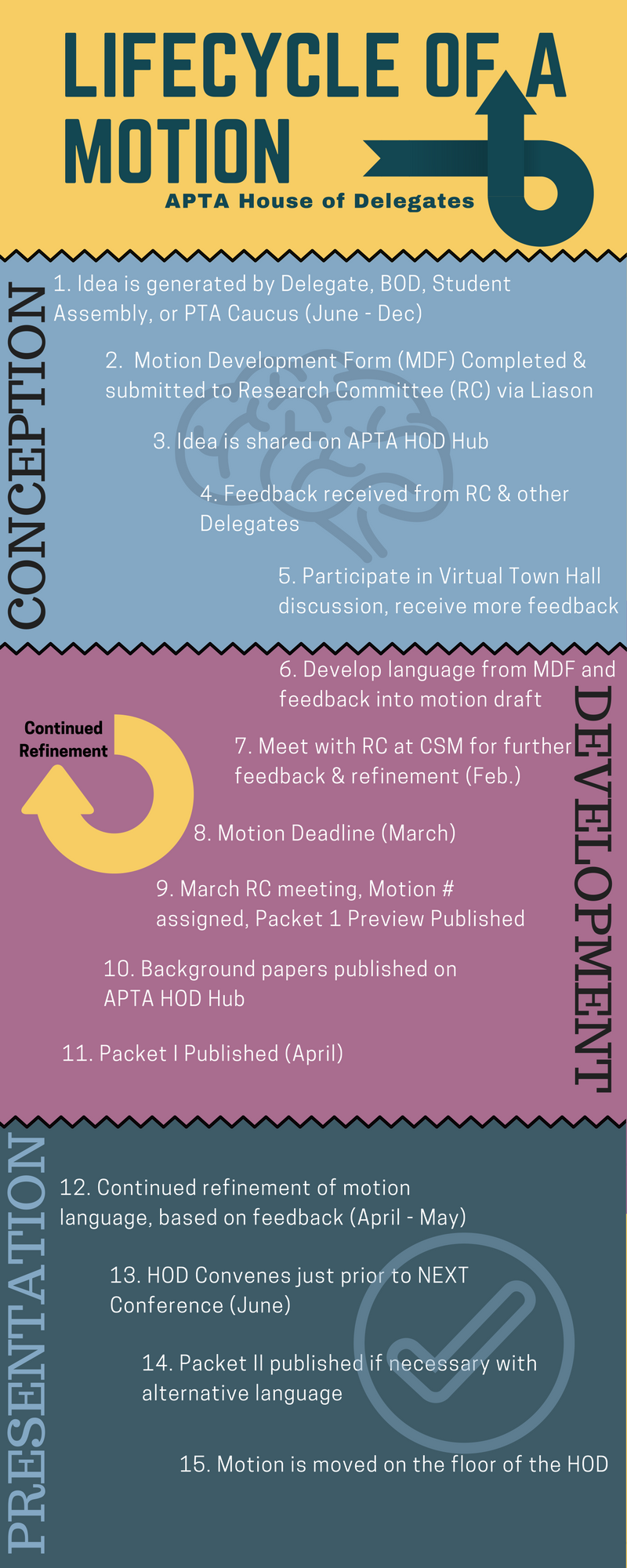
According to the APTA, all motions other than bylaw amendments, serve one of four major purposes. They define a course of action (policy), a stance (position), a binding statement to judge the quality of action (standards), or clearly state a goal the APTA wishes to achieve. Motions are vetted, researched, and revised over the course of a one or two year cycle, which typically revolves around the HOD meeting at APTA Next in June. Some more complex motions may take up to 2 years of research and refinement prior to being introduced to the House. The APTA has identified 3 major phases of the motion lifespan: Conception, Development, and Presentation.
So what does the Reference Committee do, and how many motions are introduced every year? According to Dr. Michael Pagliarulo, PT, MA, EdD, Member and former Chair of the RC, roughly 20-30 motions come before the HOD each year, but that number is decreasing as a result of considering issues of more significant impact on the profession and society. The RC’s job is not to research these motions, but to assist the delegates in the motion development process. They provide advice and counsel to the delegates on form, wording, and method of motion presentation – helping the delegates clearly state motion’s intent. This is a complex process and the RC provides the guidance necessary to the authors so it can run as smoothly as possible. And running smoothly is extremely important in this process, as Dr. Pagliarulo explains what happens once the motion is moved:
“Once motions are moved, seconded, and announced by the speaker, they become the property of the voting body. That body then debates that motion and can then vote to adopt or defeat. Amendments are also in order during the debate. The amendment can also be amended. Then you must go backwards to vote on the amendments. Once they are dispensed, other amendments are in order, and they must be voted on. Once the body has exhausted amending the main motion, then the main motion is voted on as amended, if any of them had been adopted. To make matters even more exciting, there are other types of motions that could occur during the debate. For example, the motion could be referred to the Board of Directors for further consideration, or postponed definitely to be considered after interested parties had an opportunity to meet and reach consensus on issues, or postponed indefinitely, which essentially defeats the motion. There are even other types of motions, but these are the main ones. This is why we always have a parliamentarian present at the House to help us get through some complex strategies.”
Got it? Good! Starting May 11, we will report on each of the motions that will be coming before the HOD in June. Stay tuned!
Resources:
PT Think Tank would like to sincerely thank Dr. Michael Pagliarulo for his assistance in this project.
2017 Packet I can be found here.
2017 Background Papers can be found here.
Helpful Webinars (Free to APTA members!):





