Integrating the American College of Radiology Appropriateness Criteria for Imaging for Musculoskeletal Conditions into Physical Therapist Practice
- Gail Deyle PT, DSc, DPT, OCS, FAAOMPT
- Major Michael D Ross, PT, DHSc, OCS

The presenters of this session discussed the decision making process of when a patient seen by a physical therapist may require (or benefit) from further imaging studies. They provided evidence for not only when a patient needs imaging, but what type of imaging has the best sensitive or specificity. Real patient scenarios were also presented to illustrate the decision making process, and statistics.
One of the problems that plagues physical therapy decision making in the clinical setting is the routine (and accepted!!) use of clinical tests (i.e. Homan’s Sign in screening for DVT) that actually have poor statistics and poor clinical utility. Below I will briefly summarize some of the material presented, as well as provide links to some great websites to help with a decision making process founded on proper statistical studies and grouping of findings.
Before, I get started one of the biggest take home points was a concept that is taught to all physician residents. Do not order a study or tests unless the results will alter the course of treatment or diagnosis. On a side note, I think this a concept we need to incorporate into physical therapy clinical examinations and clinical reasoning more rigorously. How many clinical tests or measures are we performing that do not alter our treatment or decision making? Major Michael Ross adapted the above principle to the physical therapist’s perspective and role in imaging:
Use imaging ONLY if a positive test will result in a change in treatment
I will expand upon this by saying that physical therapists will also be referring for imaging or further work up if they need to rule OUT a more sinister cause of the patient’s presentation before initiating, or while concurrently, initiating PT treatment. So, if you can not sufficiently rule out a DVT, fracture, or other occult pathology in your clinical examination using the best available clinical tests and statistics then we must refer that patient for further testing. Obviously, a positive test for DVT, a visualized fracture on CT, or a tumor on MR are going to change (or halt) physical therapy treatment.
Fractures
- Plain Film Radiographs: High Specificity (good at ruling in). Low Sensitivity (poor at ruling OUT)
- So, if negative plain film study, still concerned about a fracture!
- CT: High Sensitivity and Specificity. Good at ruling out and ruling in.
[Disclaimer, I have not thoroughly reviewed the statistics for overall sensitivity and specificity of plain films vs. MR for fractures OR the statistics for various body regions. But, this aligns with what I knew previously. I am presented the information as it was presented. Citations in their handouts if you have access to them. Please comment if you have references that suggest otherwise.]
Avascular Necrosis
- T1 Weighted MR is the best imaging study
- Areas of black (decreased signal) suggest AVN
Cauda Equina
- Need to be in an Emergency Department within 48 hours to prevent possibly permanent neurologic damage
- Urine retention is a specific and sensitive (.90) finding
- Saddle Anesthesia is also a strong clinical finding
Shoulder: Rotator Cuff Tears
- Fatty infiltration and atrophy on MR of the supraspinatus and infraspinatus. Poor prognosis for success with surgery.
Low Back Pain
- Only indicated when severe and progressive neurologic deficits are present
- HIGH suspicion of specific, serious pathology such as cancer, fracture, or metastases
- Correlation between pathoanatomy and function is sketcy at the absolute best
We are obviously (hopefully!!!) preaching the choir in regards to over-imaging in individuals who have low back pain. There has been an explosion of data over the past 5-10 years illustrating the presence of unnecessary and over-imaging. But, far more scary, is the findings that more imaging in low back pain is correlated with more invasive procedures and higher health costs. That is something to shoot from the rooftops: There is the potential for increased exposure to more invasive and potentially less successful treatment approaches with unnecessary imaging. Remember an image is never going to make your pain go away. One last sickening statistic. More dollars are spent each year on spinal fusions that on cancer. Here are the American College of Physicians Recommendations.
Physical Therapists can and do utilize imaging for different reasons than physicians.
Sometimes it is important to know the relevant pathoanatomy. This may guide the application of our manual therapy treatment. It may also help us make better recommendations on pursuing surgery or not. Many times we are requesting or using imaging to rule out sinister causes of a patient’s presentation.
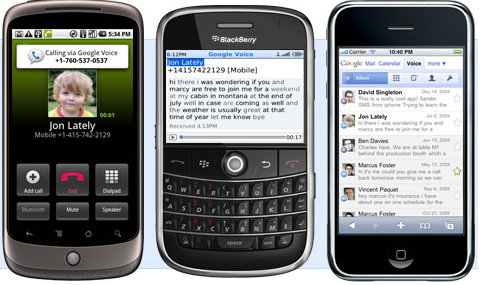
What I think is most exciting about the ACR guidelines is that they are readily available online and there is also a Mobile App!! There is also a great website, MDCalc, that integrates current evidence into decision tools that you can use instantly on the web:
- Canadian Cervical Spine Imaging Rules
- Nexus Criteria for Cervical Spine Imaging
- Ottawa and Pittsburgh Knee Rules
- Ottawa Ankle Rules
- Wells Criteria: Deep Vein Thrombosis
- Wells Criteria: Pulmonary Embolism
- National Institute of Health [NIH] Stroke Scale
As Albert Einstein said: Intelligence is not the ability to store information, but to know where to find it!
What a great way to leverage technology to utilize the best evidence for imaging and referral appropriateness. I do not think there is any data on this, but I would assume that clinicians that leverage this tools in clinical practice make better, and better informed decisions. For those of you familiar with Dr. Tim Richardson’s blog Physical Therapy Diagnosis: Make Decisions Like Doctors, he is actually developing clinical decision making support tools that can be easily integrated into EMR programs. Exciting times!!